Illustrations: Katrin Friedmann, Marta Pucci and Emma Günther
What is ovulation? Signs, symptoms, and science.
Dive into the science behind ovulation, what it feels like and how it happens.

Top things to know about ovulation
Ovulation is a major event in the menstrual cycle where a mature egg is released into your fallopian tube
There are many symptoms of ovulation, with one in five women experiencing pain
You can track your symptoms and use ovulation tests to find out when you may be ovulating
What is ovulation?
Ovulation is a major event in the menstrual cycle (1). It occurs when hormones cause the release of an egg from one ovary, into your fallopian tube (2). Like your period, the timing of ovulation can vary from cycle to cycle and differ between people (3). Research indicates that ovulation typically occurs around 500 times in your life (1) and is impacted by several factors. Factors such as the use of certain hormonal birth control pills, pregnancy, breastfeeding, and certain health conditions such as PCOS can stop you from ovulating (1,4).
How does ovulation work?
Ovulation is when a mature egg is released from your ovary. This happens around the middle of your menstrual cycle, and marks the end of the follicular phase. During this phase, your body releases a hormone called follicle-stimulating hormone (FSH).
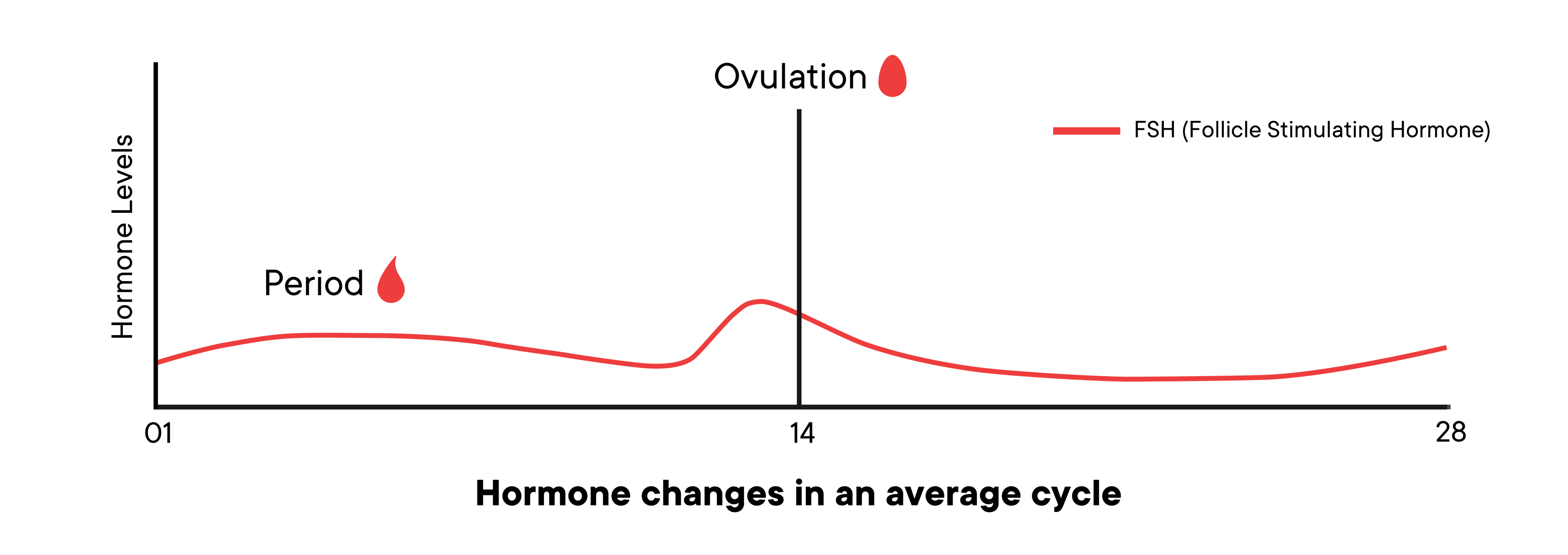
This hormone makes follicles, several small fluid-filled sacs in one of your ovaries, start to grow. Each follicle contains an immature egg known as an oocyte.
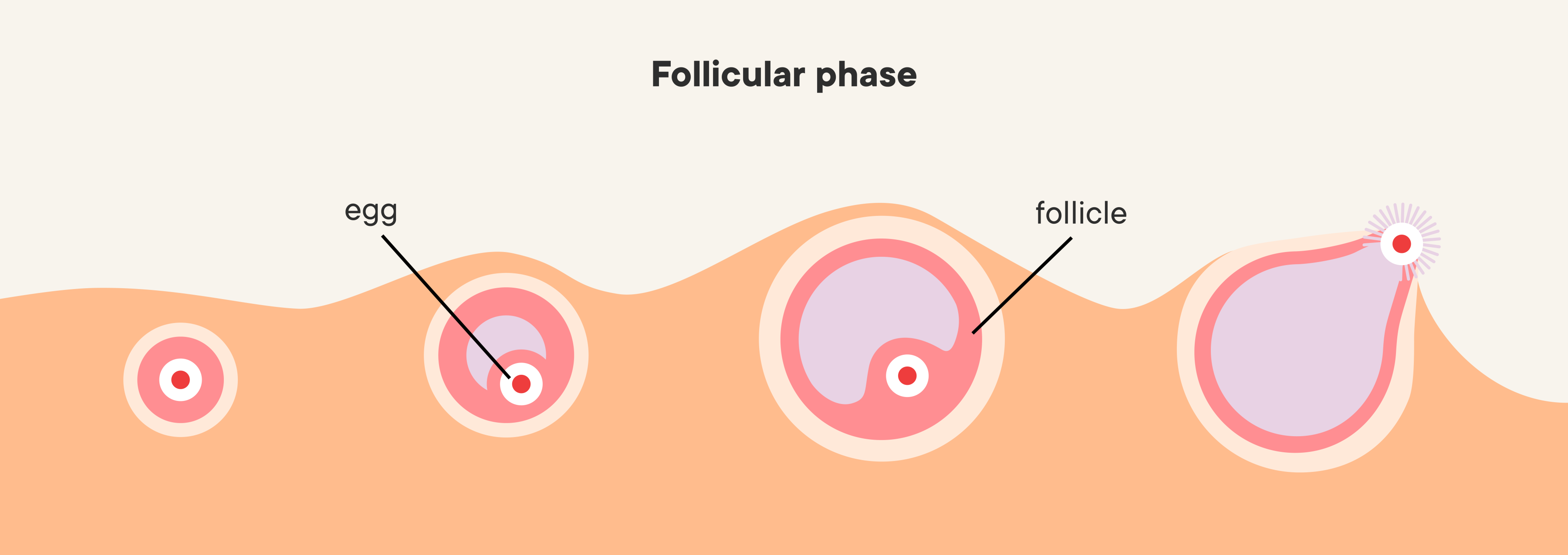
Through a series of complex hormonal changes, all but one of the follicles usually die off, generally leaving a single follicle, called the dominant follicle. When the dominant follicle is ready, another hormone called luteinizing hormone, known as LH, surges (5).
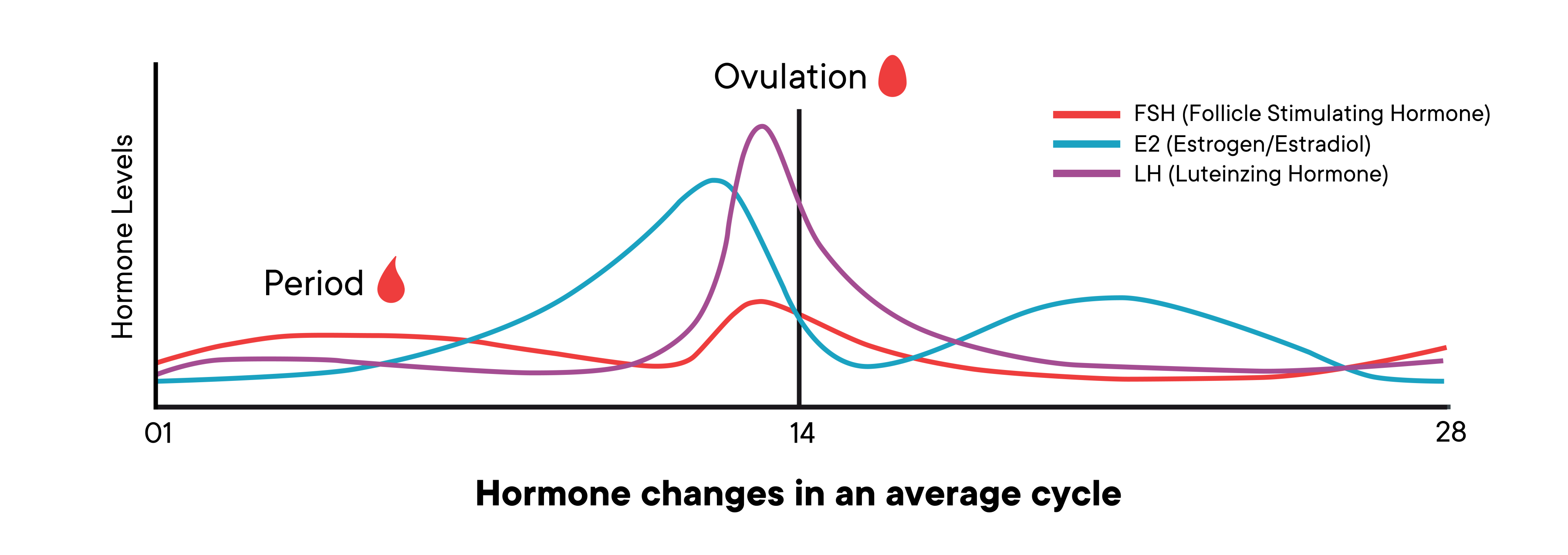
Take a look at the graph above showing how the levels of hormones change. Estrogen, in blue, starts low and begins to spike midway through the follicular phase.
This surge makes the dominant follicle burst and releases an egg. The released egg moves out of the ovary and is picked up by the fallopian tube. It is commonly thought that your right and left ovary alternate releasing an oocyte each cycle (5). The whole process usually takes about 14 days, but it can vary for each person and each cycle (1). The egg has around 12-24 hours to be fertilized by sperm in the reproductive system, where sperm can live for up to five days (1). If the egg is not fertilized, it will start to break down after around six days. If the egg is fertilized, it will travel to the uterus and possibly implant there to begin a pregnancy (1).
When does ovulation happen?
People have menstrual cycles with different lengths, therefore the timing of ovulation can vary (6). Research indicates that in a ‘typical’ 28-day menstrual cycle, ovulation is expected to occur roughly around day 14 (1, 2). Individuals also experience varying cycle lengths, meaning one cycle might be 28 days while the next could be 34 days, with variability of up to 9 days still being considered within a regular range (3,7). Generally, individuals with longer menstrual cycles tend to ovulate later in their cycle (8). If your periods are often unpredictable, it may be an indication of anovulation, where ovulation does not occur, and a reason to talk to your healthcare provider (9).
Ovulation is regulated by a series of complex hormonal changes. This means any factors affecting your body's hormones can impact ovulation, such as nutritional imbalance, stress, or excessive exercise (1). Research states that hormonal birth control, like the birth control pill, can stop ovulation from occurring by increasing progesterone and estrogen levels (10). This causes the follicles to be less sensitive to hormones, and therefore not to grow (10). Pregnancy and breastfeeding can also pause ovulation, which is due to the suppression of hormonal pathways that cause ovulation to occur (11). When you reach perimenopause, your supply of mature eggs in your ovaries diminishes and ovulation becomes unpredictable (12). When you reach menopause, your estrogen levels are low, so a mature egg might not develop, which is why ovulation normally stops (13).
What are the signs of ovulation?
There are many signs of ovulation, however, there are many people who do not experience any. Some signs and symptoms are:
Ovulation pain: otherwise known as mittelschmerz, typically begins a few years after your period starts for the first time. One in five women experience abdominal discomfort during ovulation, which can feel like mild cramping or severe pain (14).
Cervical mucus changes: a change in vaginal discharge which is normally clearer and thinner in consistency to other times during your cycle (1).
Breast soreness or tenderness: some people report breast tenderness or sore nipples around the time of ovulation (15), however, this can be a symptom during other phases of the menstrual cycle as well (16).
Basal body temperature: there is an increase in body temperature over the three days leading up to ovulation (17). Note that BBT is not considered a reliable tool when trying to conceive and is not recommended by The American Society of Reproductive Medicine.
Increased libido: an increase in your sex drive (18).
Vaginal bleeding: some people experience light spotting known as midcycle bleeding. Around 5% of people can experience a bleed in the middle of their cycle, which is around the time of ovulation (19).
Bloating: sometimes people feel bloated before and during ovulation (15), however, bloating can also occur during other times of your menstrual cycle.
Positive mood: research has shown that people report a positive mood during their fertile window (20).
Appetite changes: recent research may suggest that choices in food and appetite may be affected by hormones during ovulation, however, more research is needed (21).
How can you track your ovulation symptoms?
You can track your symptoms and activities around ovulation, and throughout your menstrual cycle, in the Clue app. Tracking when your symptoms occur and how long they last can be helpful in understanding your menstrual cycle patterns, and how they affect you. You can also bring any of this information to your healthcare provider if you ever need to seek help for your symptoms.
Clue users were most likely to track their ‘Sex life’ around ovulation in the Clue app. The second most popular category to track around ovulation is ‘Feelings’, of which the most frequently reported feeling is ‘Happy’. Find out how things change for you around this time by tracking your experiences and activities in Clue.
How many days in each cycle can you get pregnant?
While ovulation is an event, or the moment the dominant follicle is released from the ovary (22), your fertile window is the time during the menstrual cycle in which you are most likely to get pregnant.
Wondering how long you’re fertile in each cycle? Historically, research has suggested that the fertile window is around six days up to and including the day of ovulation, and extends to the next day (1). Just like the day of ovulation varies from cycle to cycle, so does the timing of these fertile days.
Pregnancy can only happen when a sperm and an egg fuse, so both must be present. Unprotected sex up to five days before ovulation can lead to pregnancy. This is because sperm can survive in the body for about five days. Sperm survival is affected by their mobility, the amount of sperm present, and the type of cervical fluid present (23).
How often should you have sex if you’re trying to conceive?
The likelihood of pregnancy during the fertile window is similar whether you have sex daily, every other day, or even every three days (24). Sperm can live for up to five days in the reproductive system, so having sex every other day during the fertile window ensures that there is always sperm available for when ovulation occurs (25). Timing sex or home insemination during certain days can increase your likelihood of becoming pregnant (26). You can use Clue Conceive to get predictions on when it’s best to try to get pregnant.
While having regular sex can increase the chances of becoming pregnant, research has shown that other factors also play a significant role. These include smoking, alcohol consumption, exercise, mental health, and obesity (27,28).
Do you ovulate every month?
The development and release of an egg each cycle occurs in response to the complex ups and downs of your reproductive hormones (1). Ovulation and the menstrual cycle as a whole are impacted by energetic, nutritional, emotional, and socioeconomic factors. Short-term factors like jet lag, seasonal changes, stress, exercise, and smoking can have an effect, as well as longer-term factors like PCOS and thyroid disorders (1,4). Any factors that influence the hormonal pulsing in your brain can influence your ovulation.
Can I track exactly when I have ovulated?
For some people, like those trying to conceive, it is important to know when you are ovulating. Among medical professionals, the ‘gold standard’ test for ovulation is transvaginal ultrasonography in combination with progesterone blood test (29), however, this is not possible for those who want to test ovulation at home. For people who want to know when they are ovulating, there are many different methods:
Paying attention to cervical mucus and discharge: As mentioned above, your discharge changes to become watery and similar to an egg white, in the days around ovulation (22). Tracking how your discharge changes across your menstrual cycle will help you to know when you are ovulating.
Ovulation Prediction Test Kits: For those who want to know when ovulation is about to occur, you can use at-home urine tests. They work by detecting the sharp rise in luteinizing hormone, right before ovulation. When used as directed, they work 9 out of 10 times (30).
Basal body temperature monitoring: As explained above, your basal body temperature changes slightly when you ovulate (17). Some people track ovulation this way, however, it is not considered a reliable tool when trying to conceive (22).
Menstrual Calendar Charting: You can also keep track of your menstrual cycle to understand your body and cycle better. When you track your period in Clue, it will calculate your estimated ovulation day. Clue has a clinically tested algorithm in Clue Conceive, that was proven to efficiently identify the fertile days of each cycle.
Despite some of these methods being useful for tracking ovulation and fertile days, they are not recommended to be used as contraception (31). If you do not want to become pregnant, speak to your healthcare provider to find the best contraception for you.
Typically, people ovulate once per menstrual cycle, however, menstrual cycles can vary significantly in length, with normal cycles ranging from 24–38 days, and a menstrual period of 8 days (32). If your menstrual cycle is consistently outside this range, it may be an indication of anovulation and a reason to talk to your healthcare provider. One study revealed that even women with regular 28-day menstrual cycles may occasionally experience anovulation (33).
Do you still ovulate when you’re on birth control?
Whether you ovulate depends on what birth control method you are using. Some birth control methods, such as the progesterone-only injection, progesterone-only implant, combined birth control pill, transdermal patch, and vaginal ring work by stopping ovulation from happening. The progesterone-only pill suppresses ovulation but does not completely stop it 100% of the time. Often, you continue to ovulate when you use birth control such as the copper IUD, or hormonal IUD, however, sometimes a hormonal IUD can stop ovulation. This means that in some months people who use this method will still ovulate while in other months ovulation might not occur. This does not affect the method's efficacy and safety in preventing a pregnancy. The copper IUD does not interfere with your hormones and has therefore no effect on your menstrual cycle, thus will not inhibit ovulation (34).
Why is ovulating a sign of good health?
The process of ovulation provides your body with much-needed levels of estrogen and progesterone—hormones that play a role well beyond fertility. They impact your bone density, heart health, metabolism, sleep quality, mental health, and beyond. Getting enough of them is important (35). Occasional anovulation is generally not a cause for concern. However, if it becomes frequent or if you stop ovulating altogether, and you are not taking certain birth control, it could lead to serious health issues. Conditions that cause anovulation, such as PCOS during the fertile years are linked to osteoporosis, cardiovascular disease, and certain cancers later in life (1). If you think you are not ovulating, it may be a good idea to speak to your healthcare provider.
Now you know more about ovulation
Ovulation is an event in the menstrual cycle where a mature egg is released from one of your ovaries. This happens at the end of your follicular phase and is controlled by a complex series of hormonal changes. Many factors can determine whether and when you ovulate, such as stress and even jet lag. Some people experience ovulation symptoms such as mittelschmerz and bloating while others don’t experience any at all. With Clue, you can track over 250 symptoms related to reproductive health. Tracking with Clue helps you understand your body better and identify when you might be ovulating. Remember, it’s not in your head; it’s in your data!
FAQs
What does ovulation feel like?
For some people, ovulation might not feel like anything. For others, ovulation can feel like mild cramping on one or both sides of the lower abdomen or severe pain in that area (13). Some people experience other symptoms such as breast soreness, increased libido, cervical mucus changes, bloating, and changes in their mood (1,16,20).
Can you get pregnant if you don’t ovulate?
The short answer is no. If you do not ovulate, you do not release an egg that can be fertilized by sperm, which is required for a pregnancy (36).
Why do I feel bloated around ovulation time?
The spike in luteinizing hormone followed by the drop in estrogen combined with a rise in progesterone around ovulation may contribute to fluid retention which can cause bloating (37). It is also common to experience bloating at other times during the menstrual cycle, like when you are on your period (38).
Why do I have cravings close to ovulation time?
Although there is no specific research to explain why you may crave certain foods during the time of ovulation, studies have shown that you may have cravings in general during different times of your cycle. One study found that women craved food such as chocolate and desserts just before their period (39). So there you have it, you’re not alone in reaching for a bar of chocolate when your period is about to start.
If I don’t feel any ovulation symptoms, can I still be fertile?
There is no research to suggest that a lack of ovulation symptoms means that you are less fertile, and many people do not experience symptoms of ovulation. However, understanding when you are ovulating may increase your chances of becoming pregnant as you can time unprotected sex around that time (40).
Article was originally published Nov. 23, 2017
