Illustrations by Marta Pucci & Emma Günther
What are the phases of the menstrual cycle?
More than just your period
Top things to know about the menstrual cycle:
The menstrual cycle starts on the first day of your period and ends the day before your next period begins
Both the uterus and ovaries experience changes throughout the cycle
Ovulation occurs when an ovary releases an egg
Hormones send signals back and forth between the brain, ovaries, and uterus to begin the cycle
Tracking your menstrual cycle with Clue can help you understand your body, predict your next period, and identify patterns
Why understanding your cycle matters
The menstrual cycle is a part of your everyday life, affecting everything from energy levels and sex drive to mood and overall health (1). Understanding the different phases of the menstrual cycle can give you deeper insights into your fertility and help you make informed decisions about your daily activities. Knowing when to expect certain changes can help you plan exercise routines, special events, or even healthcare visits with more confidence.
The menstrual cycle is more than just a period
The menstrual cycle is a chain of activities in the brain, ovaries, and uterus linked to hormones; the chemical signals sent through the blood from one part of the body to another (1). This cycle consists of two interconnected cycles running in parallel:
The ovarian cycle (changes in the ovaries)
The uterine cycle (changes in the uterus)
Although these cycles are described separately, they overlap and work together in real time.
The menstrual cycle is broken into phases
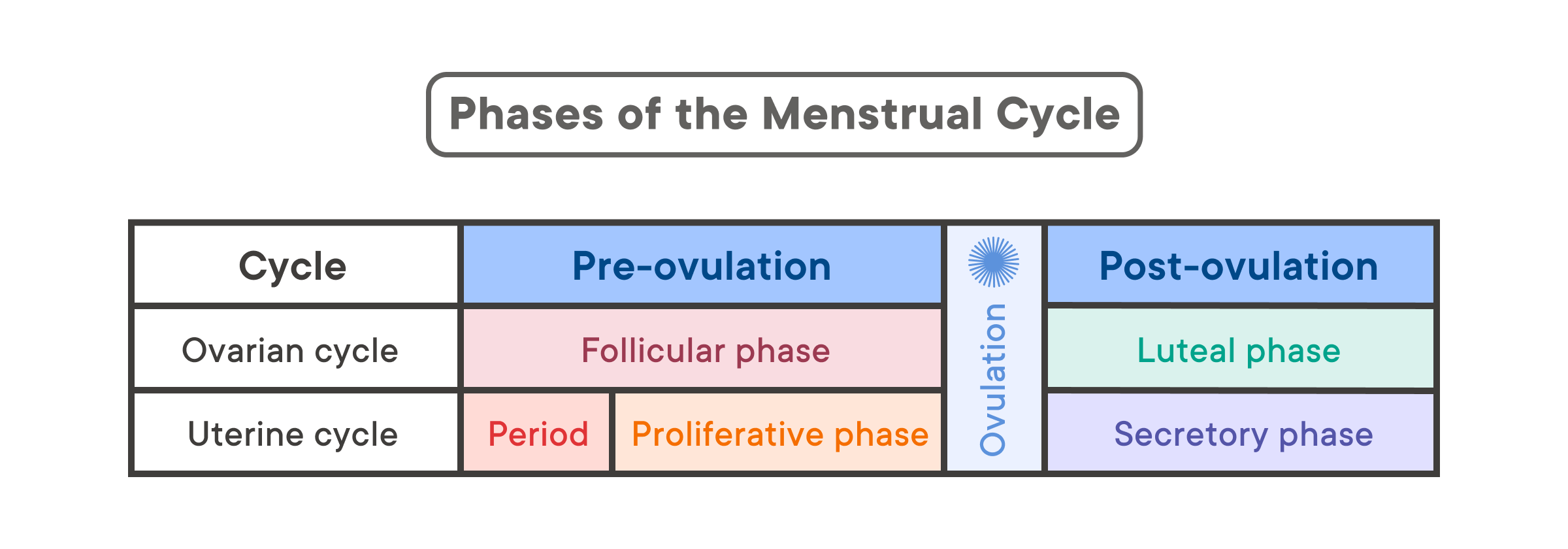
The uterine cycle and the ovarian cycle are divided into different phases—in other words, different stages (1). Different events occur during each phase. There are three phases in the ovarian cycle: follicular (before ovulation), ovulation (when an egg is released from an ovary), and luteal (after ovulation) (1). There are four phases in the uterine cycle: menstruation, proliferative phase, ovulation, and secretory (before period bleeding) (1).
Menstrual cycles vary
A menstrual cycle starts on the first day of your period and ends the day before your next period begins. One full cycle usually lasts between 24 and 38 days, but this can vary from person to person and from one cycle to the next (2). Your cycle length may also change over time—for example, during the years following menarche (your first period) or as you approach menopause (when periods stop permanently) (2,4).
Sometimes, ovulation does not happen at all, which is called anovulation (1). This is more common during the early years of menstruation and again later in life during perimenopause (the transition to menopause) (1). Anovulation can also occur while breastfeeding or due to certain conditions, such as polycystic ovary syndrome (PCOS) (1,5). In some cases, you may still experience what seems like a regular period even if ovulation did not occur, and the reason for this can be unclear (4).
Because hormone levels fluctuate throughout the cycle, some people notice changes in their hair, skin, digestion (including poop), mood, migraine headaches, or even how they experience sex at different points in the cycle.
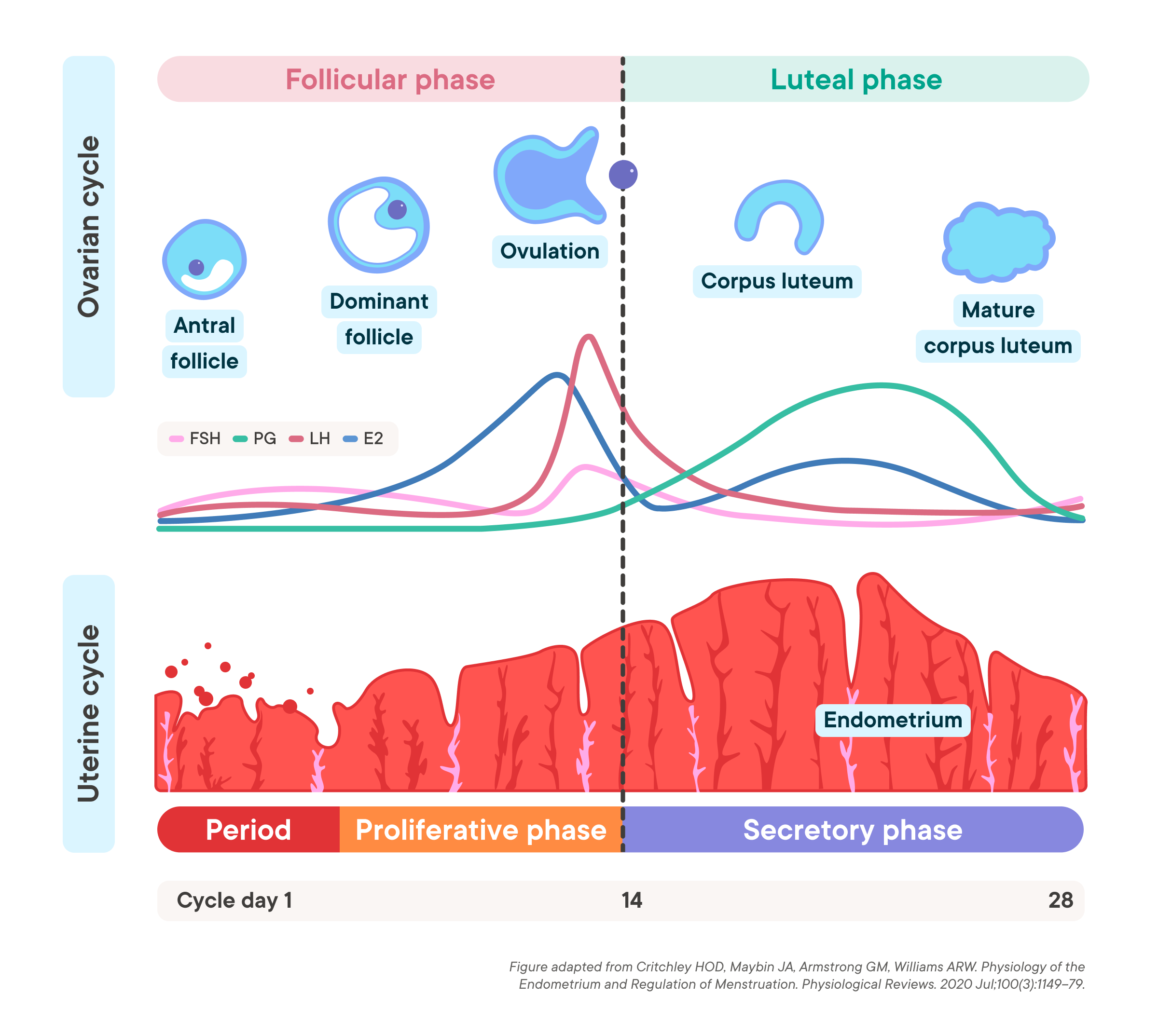
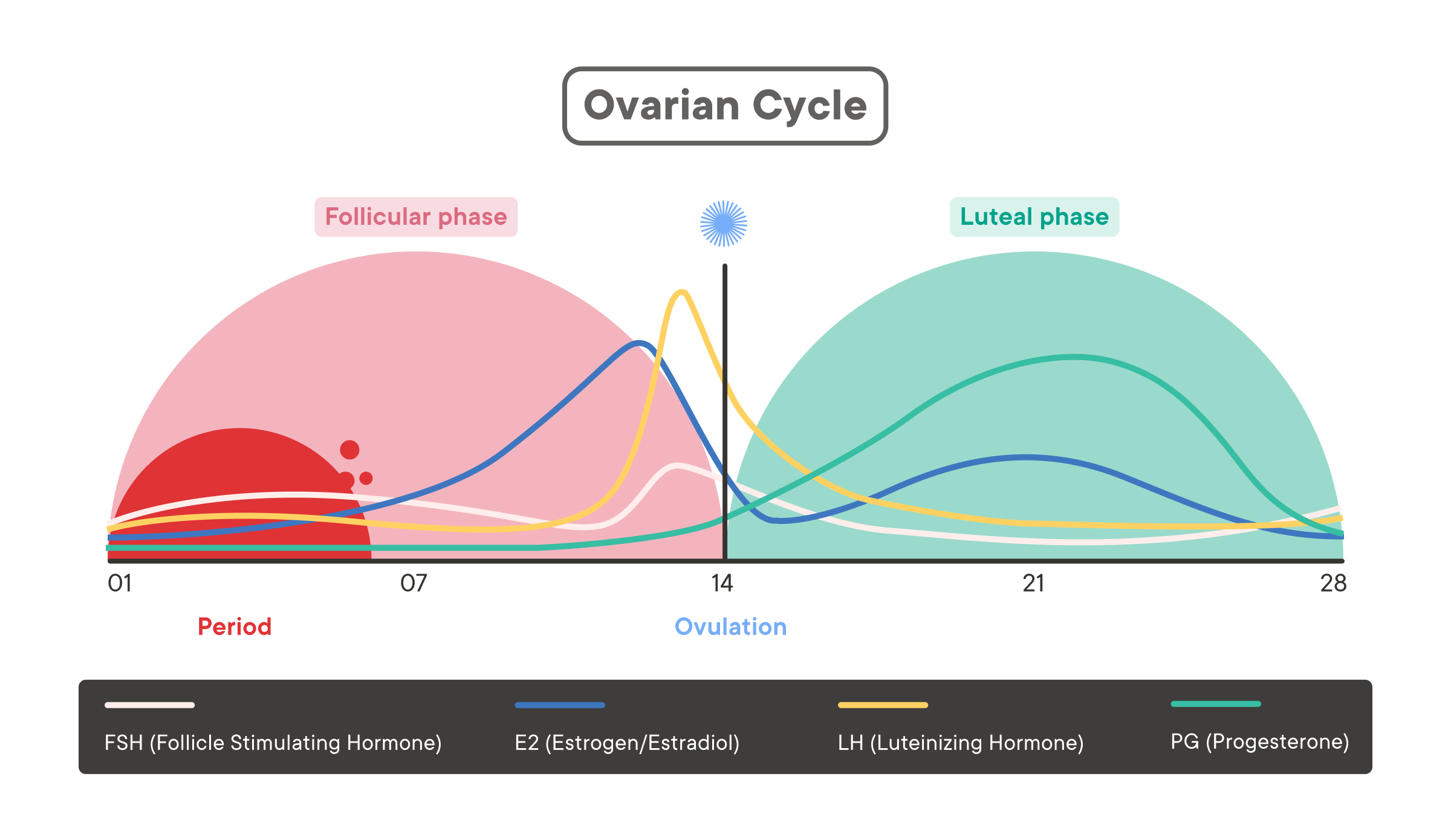
The Ovarian cycle
This cycle refers to physical changes in the ovaries.
Below, we describe an example 28-day cycle where ovulation happens on day 14. Keep in mind that cycle lengths vary, and your cycle may not follow this exact timeline.
1. Follicular phase (around days 1–14)
The most commonly tracked category in the Clue app during the follicular phase is “Sex life”, followed by “Feelings”.
When: From the start of the period until ovulation.
What: Multiple follicles (fluid-filled sacs containing eggs) develop in both ovaries (12,13). One becomes the dominant follicle, reaching about the size of the button on the front of your jeans (13,14). This follicle is the one most likely to release a mature egg at ovulation. For most people, this phase lasts about 10-22 days, but this can vary (15).
Hormones: The pituitary gland, located at the base of the brain, produces follicle-stimulating hormone (FSH), which signals the ovaries to prepare an egg for ovulation. The growing dominant follicle produces increasing estrogen levels, which peak just before ovulation (14,16).
2. Ovulation (around day 14)
(Note: Ovulation is part of both the ovarian and uterine cycles—it marks a key event in each.)
The most commonly tracked category in the Clue app during ovulation is “Sex life”, followed by “Feelings”.
When: Around the middle of the menstrual cycle, or 13 to 15 days before the start of the next period.
What: The dominant follicle releases an egg into the fallopian tube.
Hormones: A sudden surge in luteinizing hormone (LH) triggers the release of the egg (17). Estrogen levels drop right after ovulation (1).
3. Luteal phase (around days 14–28)
The most commonly tracked category in the Clue app during the luteal phase is “Feelings”, followed by “Pain”.
When: From ovulation until the start of the next period. This phase often lasts about 14 days but can range between 9 and 16 days (15,18).
What: After ovulation, the empty follicle transforms into the corpus luteum (17,19), which produces progesterone and some estrogen to support a potential pregnancy. If no pregnancy occurs, it breaks down after about 9-11 days (17).
Hormones: Progesterone (and, to a lesser extent, estrogen) rises and then falls if pregnancy does not occur (20,21). This shift in hormones during the menstrual cycle contributes to typical premenstrual symptoms like mood changes, headaches, acne, bloating, and breast tenderness. When progesterone and estrogen drop, menstruation begins again.
The Uterine cycle
This cycle refers to physical changes in the uterus.
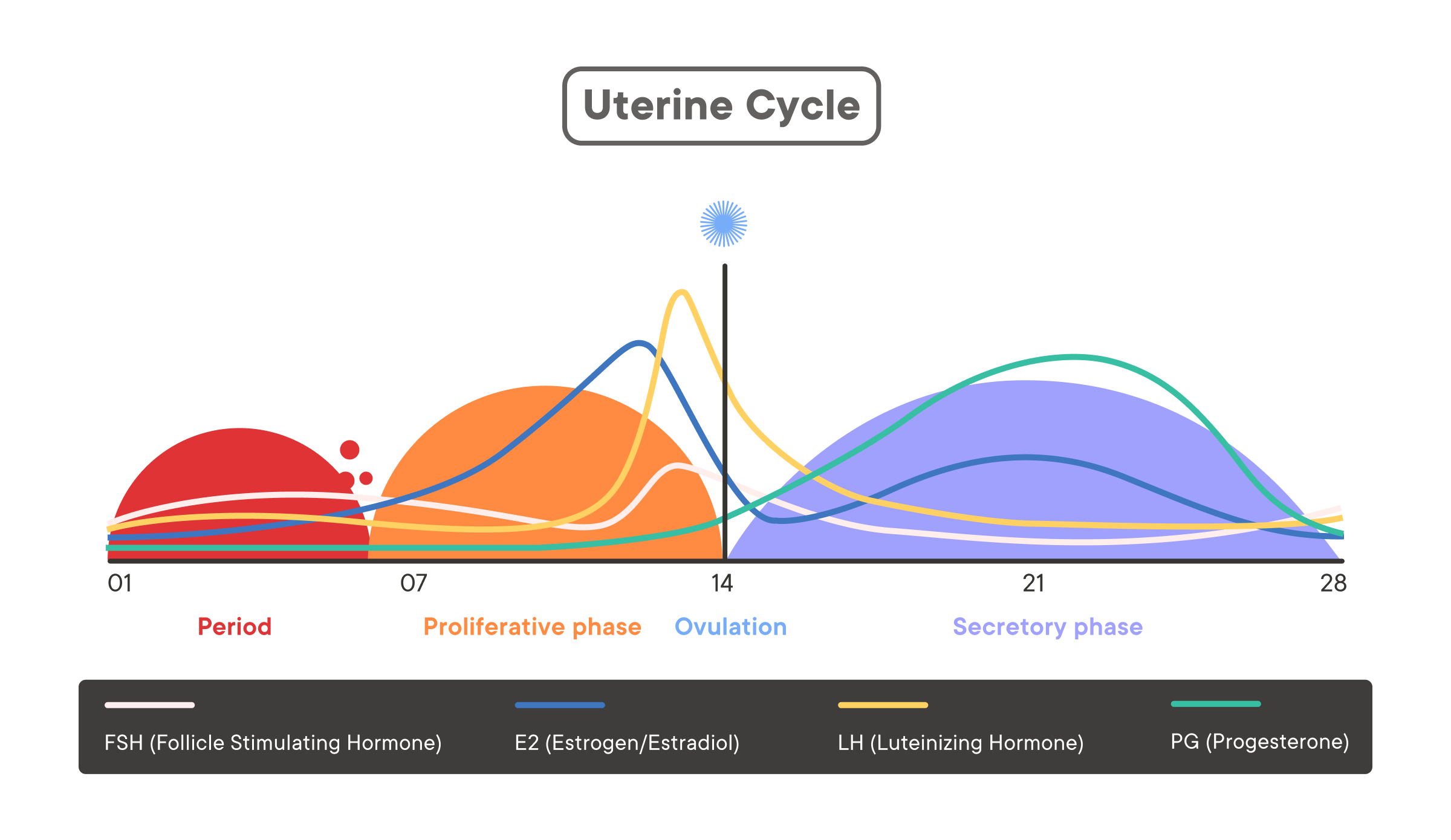
1. Menstruation (the period) (around days 1–5)
The most commonly tracked category in the Clue app during the menstrual phase (excluding “Period”) is “Pain”, followed by “Feelings”.
When: From the start to the end of the period.
What: Blood and tissue from the previous cycle’s uterine lining (endometrium) are shed through the cervix and vagina. The endometrium is at its thinnest during this phase. A typical period may last up to 8 days, but on average it’s about 5-6 days (2,6).
Hormones: Estrogen and progesterone levels are usually at their lowest. This causes the top layers of the lining to break down and leave the body.
2. Proliferative phase (around days 6–14)
When: From the end of the period until ovulation.
What: “Proliferative” means growing quickly. During this phase, the uterus rebuilds and thickens its lining to prepare for a potential pregnancy. Meanwhile, the ovaries prepare eggs (oocytes) for release (7).
Hormones: Estrogen levels typically rise during this phase. This signals the uterine lining to grow.
3. Ovulation (around day 14)
(Note: Ovulation is part of both the ovarian and uterine cycles—it marks a key event in each.)
The most commonly tracked category in the Clue app during ovulation is “Sex life”, followed by “Feelings”.
When: About midway through the menstrual cycle, or 13 to 15 days before the start of the next period.
What: The dominant follicle releases an egg into the fallopian tube.
Hormones: A sudden surge in luteinizing hormone (LH) triggers the release of the egg (17). Estrogen levels drop right after ovulation (1).
4. Secretory phase (around days 14–28)
The most commonly tracked option in the Clue app during the secretory phase is “Breast tenderness", followed by “Cramps”.
When: From ovulation until the start of the next period.
What: The endometrium becomes thicker and richer in nutrients, ready to support a fertilized egg if pregnancy occurs. If no fertilized egg implants, the lining of the uterus breaks down and your period begins.
Hormones: Progesterone rises during this phase, causing the uterine lining to stop thickening and prepare for implantation. In the late secretory phase, the body produces prostaglandins, hormone-like compounds that can cause cramps to help shed the lining if pregnancy does not occur (9-11).
Menstruation will begin again, and the cycle starts over.
When to see a healthcare provider
Some variation in the menstrual cycle is typical, but consider talking to a healthcare provider if you (2,22-24):
Consistently have cycles shorter than 24 days or longer than 38 days.
Skip periods for more than three months in a row (and aren’t pregnant).
Experience very heavy or prolonged bleeding (e.g. soaking through pads or tampons every hour for several hours or bleeding for longer than 8 days).
Have severe pain or other symptoms that affect your daily life.
You can use Clue to track your cycles and any related symptoms. Visit the “Analysis Tab” to view your cycle statistics, including cycle length, variation, and period flow. Your healthcare provider can help you determine whether your experiences are normal variations or signs of an underlying condition.
Summary
The menstrual cycle can be divided into two main processes: the uterine cycle and the ovarian cycle, which run in parallel.
The key phases of the uterine cycle are menstruation, the proliferative phase, ovulation, and the secretory phase.
The key phases of the ovarian cycle are the follicular phase, ovulation, and the luteal phase.
Hormones—particularly estrogen, progesterone, FSH, and LH—play pivotal roles in each phase, signaling the brain, ovaries, and uterus.
Real-life cycles are rarely textbook; they can vary from one cycle to the next and change throughout your life.
Tracking your cycle with Clue can help you identify patterns, predict ovulation and periods, and provide valuable information for conversations with your healthcare provider.
FAQs
What are the four phases of the menstrual cycle in order?
While the menstrual cycle is actually two separate cycles running in parallel, it is common to hear it described as four main phases:
Menstruation (the period): The uterine lining sheds.
Follicular phase (ovarian)/Proliferative phase (uterine): The follicle in the ovary prepares an egg and the uterine lining rebuilds.
Ovulation: The egg is released from the dominant follicle in the ovary.
Luteal phase (ovarian)/Secretory phase (uterine): The corpus luteum forms and releases hormones to prepare for a possible pregnancy.
How do you know what phase of your cycle you are in?
Some methods to estimate your cycle phase include (25):
Tracking the days since your last period (e.g. with Clue).
Observing symptoms such as cervical mucus, basal body temperature, or hormonal pattern changes.
Using ovulation predictor kits if you’re trying to pinpoint ovulation.
How do you feel during the luteal phase?
The luteal phase is the time between ovulation and the start of your next period. Many people experience premenstrual syndrome (PMS) during this phase, which can include a variety of physical and emotional changes (26):
Mood changes, such as irritability, sadness, or anxiety
Physical symptoms, like bloating, breast tenderness, mild cramping, and changes in appetite or cravings
Fatigue or fluctuating energy levels.
Not everyone goes through PMS, and symptoms can vary from person to person (26). You can use the Clue app to track PMS and get predictions on when symptoms may occur. If your symptoms are severe enough to interfere with your daily life, reach out to your healthcare provider.