Illustrations by Emma Günther
Estrogen 101: Levels throughout the cycle
Getting to know our hormones.

Top things to know:
Estrogen is one of the most well-known sex hormones
Estrogen levels can vary from person to person and cycle to cycle
Estradiol is the most active form of estrogen
Low estrogen can affect your physical and mental well-being
What is estrogen?
Estrogen is one of the most well-known sex hormones in women and people who menstruate. It is made in the body from cholesterol, a type of fat molecule (1).
Hormones enable cells throughout the body to communicate with each other. Cells with estrogen receptors have functions that are turned on or off by estrogen. Imagine estrogen as a key and estrogen receptors as a lock—together, they make your body systems work (2).
Estrogen is not exclusive to cis women or people who menstruate. Men, trans women, children, and post-menopausal people also have estrogen in their bodies (3). However, these people don't have ovaries that actively produce eggs each month, so their estrogen is made in other parts of the body, such as in fat tissue, bones, skin, the liver, and the adrenal glands (3). In adult men, estrogen is produced in the testes (4).
What does estrogen do for the body?
Estrogen is a key component in the menstrual cycle and plays a crucial role in the development of secondary sex characteristics, including breast development and pubic hair growth, starting at puberty (5,6). But that's not all—estrogen also influences many other functions, including bone health (7), cognitive function (8,9), cardiovascular health (10), and much more.
Types of estrogen
There are four main types of estrogen in women and people who menstruate, which serve various functions in the body depending on your life stage. For example, during pregnancy, different types of estrogen are produced to help support the pregnancy and prepare the body for childbirth (11).
Here are the four main types of estrogen:
Estrone (E1): This is a weak form of estrogen, mainly produced in body fat, but also in the ovaries and placenta (2,11,12).
Estradiol (E2): The most active type of estrogen, this is the type involved in the menstrual cycle (2,11). Estradiol (E2) binds very strongly to the estrogen receptors. When we talk about “estrogen” at Clue, we are almost always talking about this type.
Estriol (E3): This is the main type of estrogen made during pregnancy, mainly made and released by the placenta. It is also a weak estrogen (2,11).
Estetrol (E4): A type of estrogen that is only produced during pregnancy by the liver of the fetus (2,11).
Weak estrogens can attach to estrogen receptors, but their effect on the body is less dramatic than that of more active estrogens. In other words, they are not as potent as the stronger forms of estrogen.
Most of the estrogen in the body is estradiol and it’s made in the ovaries. However, estrogens are also made in other parts of the body, including fat tissue, bones, skin, the liver, and the adrenal glands (3). As people go through menopause, these other sources of estrogen increase their production and become more influential in the body (13).
How does estradiol (E2) change during the menstrual cycle?
Do you remember how the menstrual cycle works? Like a relay race, many different hormones are involved in the maturing and releasing of eggs to prepare the body for possible fertilization and implantation. Estradiol is one of the main players.
Stage 1: Follicular phase = increasing estrogen
Estradiol is mainly produced in the ovaries. During the first part of your cycle—from the start of your period until ovulation (the follicular phase)—estradiol is made by the sacs that contain your eggs, called follicles. Estradiol stimulates the growth and thickening of the endometrium (the lining of the uterus) (2).
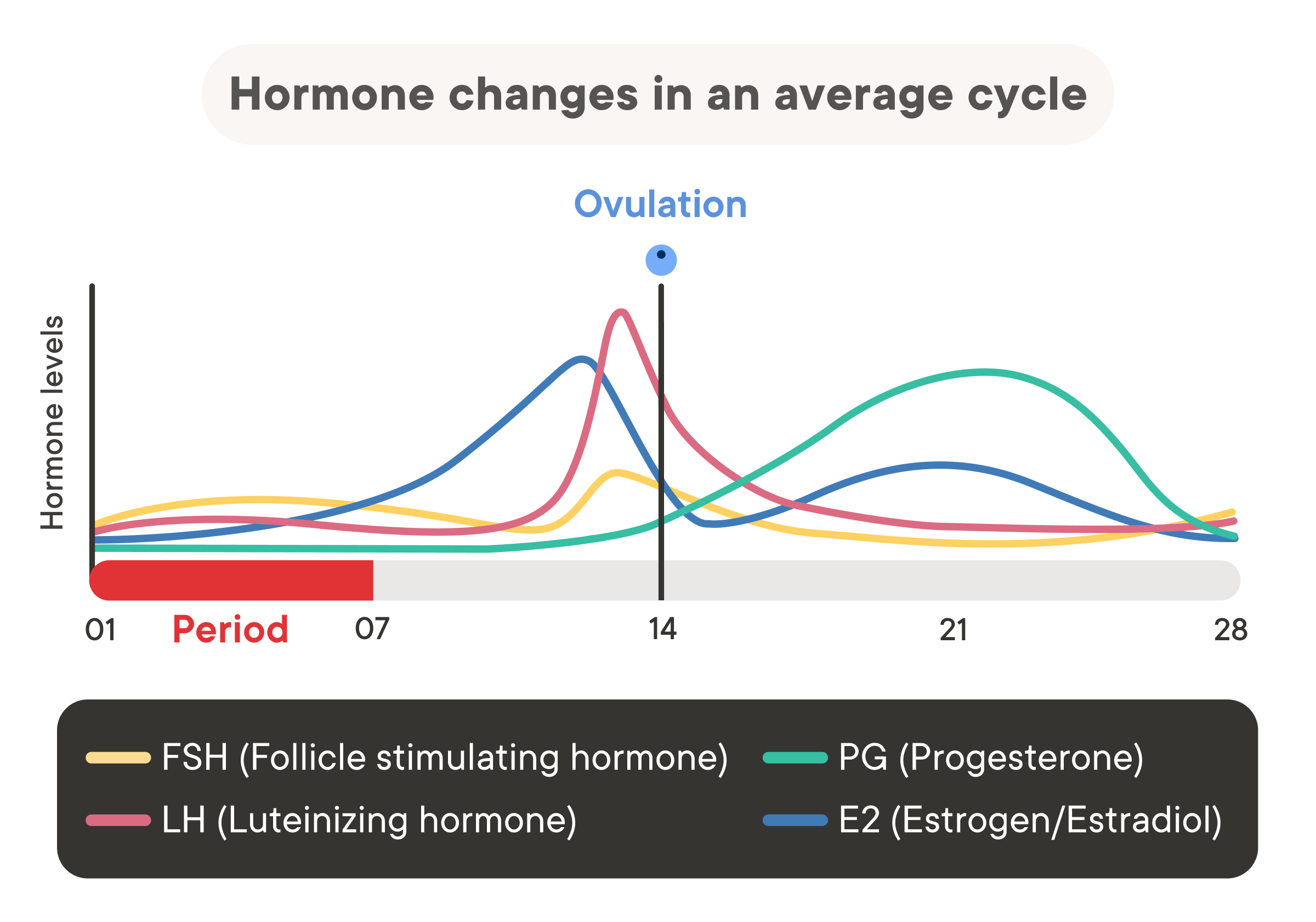
Towards the end of the follicular (first) phase, estradiol levels peak and trigger the brain to release two hormones: a large rise in luteinizing hormone (LH) and a smaller rise in follicle-stimulating hormone (FSH) (2,14). This then triggers ovulation. Just before ovulation, the follicle stops producing estradiol, causing the levels to drop (2).
During this phase of your cycle—from the start of your period to ovulation—estrogen levels are high. You may notice some changes in your body. Just before ovulation, some people notice that their skin and hair are less oily, although we don't know for sure that the increased estrogen causes this (15).
Your cervical fluid also changes throughout the follicular phase:
Early to mid follicular: dry/sticky
Mid to late follicular: thick/sticky/creamy
Late follicular to ovulation: wet and slippery, like egg white (2,16)
Additionally, some people notice an increase in their sex drive around ovulation (17-19)
Stage 2: Luteal phase = lower levels of estrogen
About halfway through the cycle, the follicle ruptures and releases an egg (ovulation), and the luteal phase begins. After the egg is released, the follicle’s walls form a new structure called the corpus luteum. The main function of the corpus luteum is to produce high levels of progesterone and some estradiol (2).
If an egg is not fertilized and implanted, the corpus luteum stops producing progesterone and estradiol about four days before menstruation starts, and the levels of both hormones in your blood fall again. This triggers the start of your menstruation (2).
When estrogen levels are lower—such as before your period, during the late luteal phase, and at the start of your period—you may notice some of these changes:
A rise in your overall body temperature.
Increased skin sensitivity: A study found that 2 out of 5 women reported more sensitive skin, which researchers think may be due to the lower estrogen levels (20).
Premenstrual symptoms (PMS): This can occur during the time before your period starts when estrogen (and progesterone) levels are low.
Migraines: Menstrual migraines are also linked to the drop in estrogen levels (21,22).
What are “normal” levels of estrogen during your cycle?
Estrogen levels fluctuate greatly throughout the cycle. A “normal” level of estrogen varies per day unless you are on hormonal birth control, which stabilizes hormone levels.
If you’re experiencing unexpected symptoms and suspect that your estrogen is high or low, you can ask your healthcare provider to run tests. Estrogen levels fluctuate throughout the menstrual cycle and can also vary from one cycle to another. As a result, it's possible to have different test results when estrogen is measured multiple times (23).
Differences in laboratory procedures, population served by the laboratory, and testing technique can also impact results, so lab results should always be interpreted using the lab’s reference values (22).
Estrogen levels in people with regular cycles (not using hormonal birth control)
Estradiol levels in the blood can range considerably across the cycle. What’s considered “normal” can vary based on the lab you go to, where you live, your ancestry, and the testing technique. So you should always interpret your lab results with this in mind, but you can also use the following reference points:
Early follicular phase: 20-80 pg/mL
Midcycle peak: 200-500 pg/mL
Luteal phase: 60-200 pg/mL
Before puberty and after menopause estradiol levels are generally below 20 pg/mL (24). Estrogen levels can also differ dramatically from cycle to cycle and from person to person (23).
Estrogen levels during pregnancy
Hormone production is particularly high during pregnancy. Estradiol rises sharply, along with other hormones such as progesterone, testosterone, and prolactin (23). These hormones and many others work together to support the development of the fetus. You can use the following reference points:
First trimester estradiol: 188-2497 pg/mL
Second trimester estradiol: 1278-7192 pg/mL
Third trimester estradiol: 3460-6137 pg/mL (23)
Estrogen levels during perimenopause and menopause
After menopause, estrogen levels drop significantly because there are fewer follicles in your ovaries. In addition, these follicles no longer grow and do not produce the estradiol surges that occur during the menstrual cycle (2). Laboratory estradiol levels in postmenopausal people are usually less than 20 pg/mL (73 pmol/L) (25).
In the years leading up to menopause, known as perimenopause, people may notice that their bodies change in response to these lower levels of estrogen.
Symptoms of low estrogen in perimenopause and menopause can include:
Vaginal dryness (known as atrophic vaginitis or vulvovaginal atrophy): Without enough estrogen, the walls of the vagina are unable to maintain their thickness and are less moist (26).
Hot flashes: These are associated with falling estrogen levels and can be treated with estrogen therapy (27). Phytoestrogens, or estrogens from food, may have some benefits, but more research is needed (28).
Risk of osteoporosis: A condition in which bones become weaker and more likely to break, due to a reduction in estrogen levels (29).
How can I tell if my estrogen levels are normal?
Many physical symptoms can help tell you whether your hormone levels are within the normal range. A lack of typical development during puberty, an “irregular” menstrual cycle, or infertility (difficulty falling pregnant) can all point toward a possible underlying hormonal issue.
Estrogen levels (along with all the other sex hormones) fluctuate throughout the menstrual cycle and life. For most people, these changes are normal and part of aging.
Perimenopause, in particular, can be a wild hormonal ride, leading to unexpected symptoms at inconvenient times, like hot flashes, trouble sleeping, and unpredictable periods. Some people choose hormone therapy to help control these symptoms (29).
What is estrogen dominance?
You may have heard of “estrogen excess” or “estrogen dominance,” and how it can affect your cycle. This describes a situation where there is too much estrogen in your body, beyond what is considered within range (30).
Estrogen levels can be too high as a result of a medical condition. For example, rare genetic conditions and some cancers can cause elevated estrogen levels (31,32).
If you’ve read about estrogen imbalances on health blogs, they do not usually focus on rare genetic conditions or cancers. These blogs typically discuss hormonal imbalances caused by diet, use of hormonal contraceptives, or body fat.
One cause that is often discussed is an imbalance in the levels of estrogen and progesterone— where estrogen levels can stay high whilst progesterone levels fall.
Another proposed cause is an imbalance between the different types of estrogen. These imbalances are not usually seen as independent conditions in general medicine but may indicate another underlying issue.
Unpredictable or missed menstrual periods, along with normal or elevated E2 (Estradiol) levels and often high E1 (Estrone) levels, may indicate polycystic ovarian syndrome (PCOS), an underlying medical condition. Further testing, such as blood work and imaging, may be needed to confirm (33).
Some alternative practitioners may diagnose these imbalances as independent conditions, whereas general medicine does not. However, there is little research to support these diagnoses as independent conditions.
It is common to hear that estrogens from our food, products, and environment can affect our hormone levels. Many medical organizations recognize that environmental chemicals, such as bisphenol-A (BPA), can harm the body by interfering with hormone function (34,35).
Managing “excess estrogen”
Bloggers often suggest changing your diet to manage "excess estrogen," recommending more organic vegetables and fruit, less meat and dairy, and fewer processed foods. While a healthy diet is beneficial, it’s unclear whether these changes affect estrogen levels, or whether improvements come from just eating healthier.
Also, one person's healthy diet may not be the same as another's, so it's important to listen to your body and find a diet that works for you (34,35).
If you think there may be a problem with your hormone levels, talk to your healthcare provider about checking your sex hormone levels. Estrogen is usually measured by blood tests, but urine, saliva, and even amniotic fluid tests are also available (25).
Be sure to track your cycle in Clue before you go to your appointment. This will give your healthcare provider information about your previous cycles to help them interpret your test results.
How does hormonal birth control affect estrogen levels?
Combined hormonal contraceptives (the pill, the patch, the ring)
These types of contraceptives contain both estrogen and progestin in different amounts and combinations. Many combined oral contraceptives contain ethinyl estradiol, a synthetic estrogen. In the United States, ethinyl estradiol doses do not exceed 50 mcg (36) and are often lower, as low as 10 mcg (16).
When taken as prescribed, the contraceptive pill works by interfering with the normal communication between the brain and the ovaries, so that:
Hormonal fluctuations of the menstrual cycle do not happen (16).
Follicles are less likely to mature to their final stage, which means less natural estrogen is produced (37).
Ovulation does not occur (16,38).
By stopping follicle growth and ovulation, the natural production of estrogen (and other hormones) is affected and may be responsible for any side effects or changes you experience after starting the pill (16).
The vaginal ring provides a much lower dose of ethinyl estradiol (15 mcg per day) (39). The patch provides 20 mcg (40).
Progestin-only contraceptives (IUDs, the shot, the mini-pill, etc.)
There is no estrogen in progestin-only contraceptives. These include the progestin-only pill (the mini-pill), the shot, the implant, and hormonal IUDs.
Using progestin-only contraceptives may affect the fine balance and complicated interactions of hormones involved in the menstrual cycle. Sometimes, when one hormone level is changed, there is a ripple effect that affects other hormones, including estrogen. This can cause changes in your body or your menstrual cycle, such as unpredictable bleeding, headaches, or breast tenderness. Each type of progestin-only contraceptive may have a different effect on you and your body, and some of these changes may be the result of different levels of estrogen (16,41,42).
The mini-pill
Depending on the type of progestin used and the dose in the pill, ovulation is not consistently stopped (16,41). How the mini-pill impacts natural estrogen levels is not well understood, and more research is needed.
The hormonal IUD
Hormonal IUDs are available in different progestin doses and usually do not stop ovulation. Whether ovulation (and thus estrogen production) stops depends on the progestin dose in the IUD and how long the IUD has been in place (16). Ovulation is not suppressed in most cases (16,43,44).
The contraceptive injection (shot)
The contraceptive injection works by preventing ovulation and suppressing communication between the brain and the ovaries. Estradiol levels are much lower for people using the shot, about 15 pg/mL, though this can vary from person to person (45).
The implant
The implant does not dramatically change estradiol levels (46,47). After insertion, there may be a moderate decrease, but levels slowly rise to the pre-insertion levels (or close to them) over 2–3 years (46,47).
Non-hormonal birth control
Non-hormonal contraceptives like condoms and the copper-IUD will not impact your natural hormonal fluctuations and estrogen levels (16).
Download Clue to track your menstrual cycle and related experiences, and learn about your body.
FAQs
What are the possible signs of low estrogen?
Low estrogen levels can lead to vaginal dryness, discomfort, and decreased sensitivity, which can contribute to reduced sex drive (48). Low levels may also cause hot flashes and night sweats, which can affect sleep quality (49). Some people with low estrogen levels, like during perimenopause, may experience mood swings, depression, or anxiety. In these cases, estrogen-containing medication may help relieve symptoms (50). There also appears to be a link between low estrogen levels and an increased risk of obesity and osteoporosis (51,52).
Is it better to have high or low estrogen?
What is considered "better" depends on individual circumstances. Both low and high estrogen levels carry risks. While low estrogen levels can cause symptoms such as vaginal dryness or osteoporosis, high levels can increase the risk of unpredictable bleeding, mood swings, headaches, blood clots, and cardiovascular disease (51-53). The same is true for fertility—both low and high estrogen levels can affect the possibility of falling pregnant and pregnancy outcomes (54).
