Art direction by Marta Pucci. Photography by Natalie Rose Dodd.
Vaginal dryness: Why it happens and what you can do about it
What is vaginal dryness and what can you do about it

Top things to know about vaginal dryness:
Vaginal dryness can have physical and/or psychological causes
Symptoms of vaginal dryness include pain during sex, burning vaginal or urinary sensation, or vaginal itchiness
Vaginal lubrication is often closely tied to levels of the hormone estrogen, which changes throughout life
Medications (including hormonal birth control) may cause vaginal dryness
You can have a fulfilling sex life even if you are experiencing vaginal dryness
Vaginal dryness can happen to women of all ages. Whether you’re feeling uncomfortable or just curious to learn more, it is important to know that vaginal dryness is common and there are simple ways to manage it. Read on to find out what causes it and how you can find relief.
The vagina is a lubricated environment, which means fluids are produced to minimize friction. The fluids, or secretions, protect the vagina against infections such as vaginosis and yeast infections (1,2). The processes that keep the vaginal tissue healthy and lubricated are related to the production of the hormone estrogen (1,3,4).
Vaginal dryness isn’t defined by a healthcare provider, but by you, if your vaginal dryness adversely impacts the activities and quality of your daily life. Symptoms may include a burning vaginal or urinary sensation, vaginal discomfort or itching, atypical vaginal discharge, or pain during sex or masturbation (4). Studies show that more than half of postmenopausal women and almost 1 in 5 premenopausal women experience vaginal dryness (4).

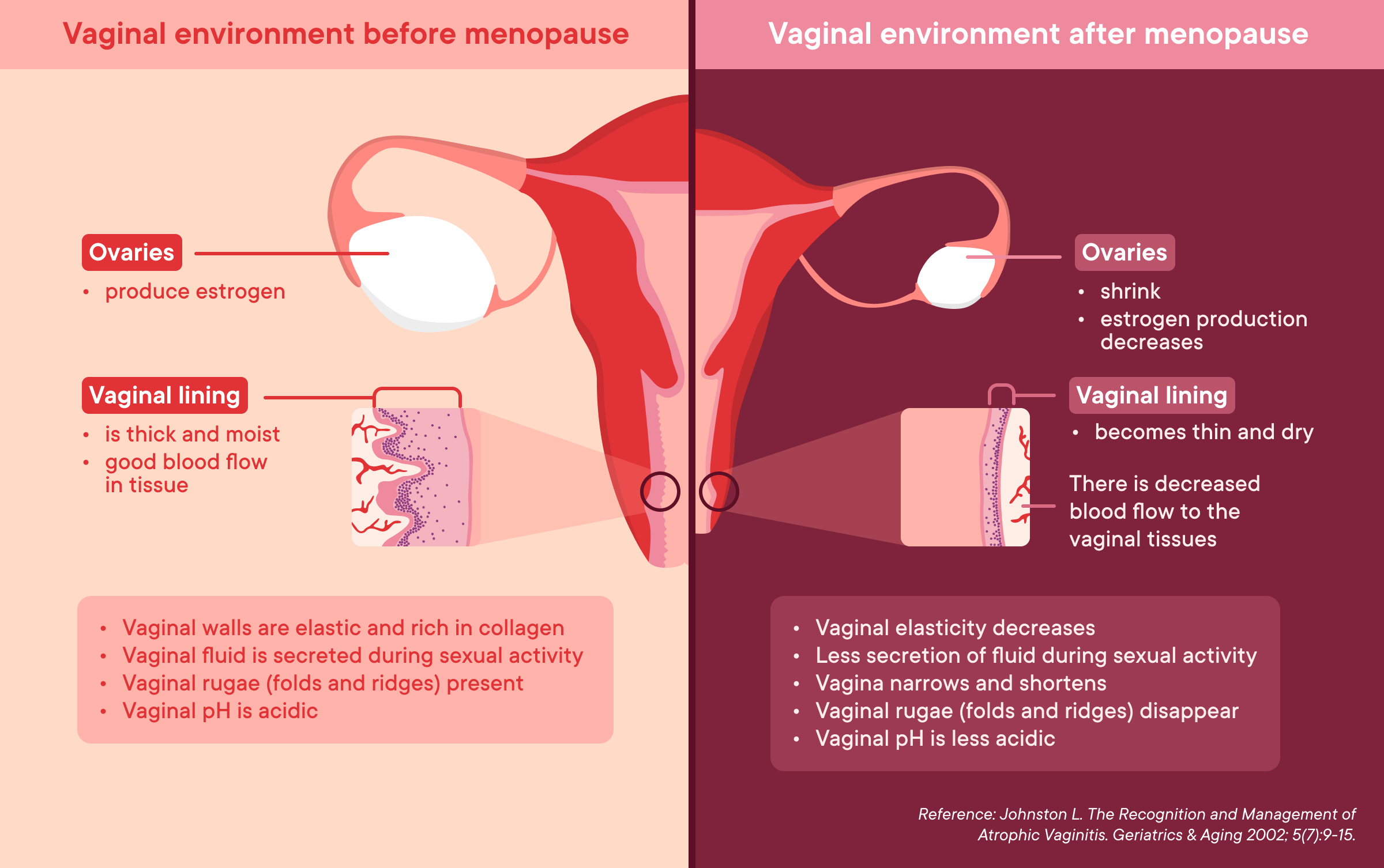
Many factors can impact your hormonal balance and contribute to vaginal dryness, such as age, life stages, mental health, chronic conditions, and medication (4,5). The ovaries produce estrogen, but when estrogen production is reduced for any reason, it can cause the vaginal lining to become thinner and dryer (5,6). This is noticeable when you are preparing to have sex or masturbate. Typically, the glands around the vagina will release lubricant secretions, also called arousal fluid, when you are ‘turned on’. A reduction of estrogen, as well as your mental health, can affect when and how much arousal fluid your body makes (3).
Vaginal dryness presents differently for different people. Some people may experience mild discomfort, others may experience extreme pain. Let’s take a deeper look at the causes and solutions (4).
Why is my vagina dry? Common causes of vaginal dryness
Reduced estrogen is the main cause of vaginal dryness
The hormone estrogen helps keep the vagina moist and maintains the thickness of the vaginal lining. When, for some reason, your estrogen levels are low, for example after giving birth or having your ovaries removed (4,8) the amount of lubricant produced reduces and the vaginal tissue gets thinner and more fragile (7). This is known as atrophic vaginitis or vaginal atrophy.
How can perimenopause and menopause affect vaginal dryness?
As perimenopause begins, the ovaries produce less estrogen, impacting the entire body. In the vagina, the lower estrogen levels cause the blood flow to the vagina to decrease and the vaginal tissue to become thinner. This can cause genitourinary syndrome of menopause (GSM), a condition that causes vaginal dryness and discomfort, pain during sex, a need to pee frequently, inability to stop a sudden urge to pee (incontinence), frequent urinary tract infections (UTI), and a smaller labia (6). As another consequence of the lower estrogen levels, the vagina also gets shorter and narrower, causing or worsening discomfort (6,7,8,12). The reason the vaginal canal becomes shorter and more narrow is because the vaginal rugae (folds of tissue), disappear progressively (13). In addition to becoming dryer, the vagina also becomes less acidic after menopause (14), and the vaginal elasticity decreases (15). In the illustration below, you can see how menopause and the reduction of estrogen affect the vaginal environment.
Which medications can cause vaginal dryness?
Hormonal birth control impacts the amount of the hormones estrogen and progesterone in your body (9). Instead of your body producing hormones that rise and fall throughout your menstrual cycle, the hormones in your birth control pill will maintain a mostly steady level. Some people may experience vaginal dryness and decreased libido when taking birth control, but research shows mixed results (9). If you experience pain during sex or have a low libido, talk to your healthcare provider to discuss which birth control method is the best fit for you (9).
Other drugs, such as antidepressants and medicine for colds, can also impact vaginal lubrication and cause vaginal dryness (2,11). You may need to review your medications with your healthcare provider, including your birth control method, if you are noticing that they are affecting your vaginal health (9,10).
You can track your medications and vaginal dryness in Clue. Tracking your medications, when you take them, and whether that coincides with vaginal dryness, can empower you with knowledge when discussing treatment options with your healthcare provider.
How can my emotions impact my sexual desire and vaginal lubrication?
Your physical and mental health can greatly influence your libido and lubrication. There are several reasons why you might notice dryness during vaginal sex. Ask yourself, are you turned on by how you and your partner are interacting? Do you feel safe? What needs to change to make sex more pleasant for you?
If you feel turned on but are still dry, your body may simply need time to catch up with your brain or you can try using lube. Talk with your partner about increasing the amount of foreplay. Take some time to think about your own sexual health. If something doesn’t seem right to you, it probably is not right. If you have vaginal dryness and lack of sexual desire, you may be experiencing low libido, and it could be caused by many factors, including medication and health conditions (9,11).
How can my menstrual cycle affect vaginal dryness?
The hormones estrogen and fluctuate throughout your menstrual cycle. These hormones also affect sexual desire. Vaginal dryness may increase in the second half of your cycle when estrogen levels are lower (4,16). Exactly how reproductive hormones influence the vagina and sex drive isn’t the same for everyone (16). Tracking your sexual desire with Clue can help you discover what’s typical for you.
Can health factors influence vaginal dryness?
Your vagina is a self-cleaning and balanced environment. Soaps, lubricants, hygiene products, internal washes (douches), or vaginal deodorants can negatively impact your vaginal health. Research has linked the practice of douching with an increased risk of bacterial and yeast infections, pelvic inflammatory disease, cervical cancer, increased transmission of sexually transmitted infections (STIs), upper genital tract infections, endometritis (inflammation of the lining of the uterus), and other adverse health outcomes (2,17,18). These conditions can affect your vaginal lubrication and sexual desire.
There is a condition where the body’s glands cannot produce enough moisture, called Sjögren’s syndrome (4,11). To keep their mucosa, such as eyes, mouth, and vagina, moist, people will need artificial products.
What can I do about vaginal dryness?
There are various treatments for vaginal dryness:
Vaginal dryness caused by low estrogen levels can be treated with several different methods: vaginal moisturizers or lubricants, local vaginal estrogen cream or tablets, systemic estrogen (and progesterone if needed) therapy, or selective estrogen receptor modulators (SERMs) (6). Speak to your healthcare provider to find the best option for you.
For dryness caused by a medication, talk to your healthcare provider about trying another medication or ways to treat the dryness while on the medication.
If what your sexual partner does during sex doesn’t work for you, try discussing your sexual preferences with them. You may find that talking about it increases your arousal. If you lack the desire to have sex with your partner, you may want to re-evaluate your relationship or talk to a healthcare provider about any health issues affecting your libido. Spending more time on foreplay can be a way to increase your natural lubrication. Another option is to use lube during sexual activity or masturbation (12).
Sexual health is complex. An answer for one person may not be the answer for another. Reach out to a healthcare provider to discuss how your physical, mental, and emotional health could impact your vaginal dryness and sexual satisfaction (12). Other professionals that may help could be a sex therapist or a pelvic floor physical therapist (12).
Personal lubricants can make sex feel better. Using lubricant can increase sexual pleasure and satisfaction in both solo masturbation and partnered sexual activities (19). Lubricants made with water or silicone can be safely used with latex condoms and diaphragms (20).
Oil-based products, such as petroleum jelly, baby oil, mineral oil, or vegetable oils, are not recommended and are likely to damage latex condoms and/or diaphragms. This increases your risk of pregnancy or STIs. Hand or body lotions are not recommended either, as they can irritate vaginal tissues (18).
Understanding the causes of vaginal dryness and taking steps to treat it can lead to a more fulfilling sex life, whether with another person or on your own. Download Clue to track your vaginal dryness, medications, and sex drive to learn more about how your menstrual experiences change throughout your cycle, or whether medications have an impact on your life.
Article was originally published on Oct. 13, 2017.
