Illustration by Emma Günther
The future of HPV screening: How self-collection tests can help eliminate cervical cancer
Clue interviews Danielle Pipher Clement, an expert in women’s health and cancer prevention
This article was created in partnership with BD, with Clue retaining full editorial authority. This content was not funded by BD, and no payment was involved in its creation.
Clue sits down with Danielle Pipher Clement, Nurse Practitioner and Women’s Health Clinical Manager at BD, to discuss the role of HPV screening in preventing cervical cancer. With her wealth of experience in both clinical practice and public health initiatives, Danielle is passionate about empowering individuals to take control of their health.
In this conversation, Danielle emphasizes the importance of raising awareness about routine HPV screening and its role in preventing cervical cancer. She also explains how HPV self-collection tests can help overcome barriers to screening, making cervical cancer prevention more accessible for some. We also touch on the potential for self-collection tests to become available for home use in the future, and how apps such as Clue, can support you through the process.
Need more information on HPV and its link to cervical cancer? Read our article: What are the differences between a pelvic exam vs a Pap smear?
Let’s dive in!
Can you explain what HPV is and why screening is so important for preventing cervical cancer?
Danielle: Human Papillomavirus (HPV) is a very common sexually transmitted infection that most people will get at some point. More than 8 in 10 women and 9 in 10 men will have it in their lifetime (1). There are over 200 types of HPV, and most of them clear up on their own without creating problems. But certain types, like HPV 16 and 18, can stay in the body and cause changes to the cervix that can lead to cancer if not detected early (2).
The problem is that HPV doesn’t always show symptoms, so many people don’t realize they have it until those changes to the cervix happen. Cervical cancer is one of the few cancers we can prevent through regular screening, which allows us to catch it before it develops. The challenge is that many people don’t fully understand how HPV causes cervical cancer, and that screening is key to catching it early.
When we think of STIs, usually the likes of chlamydia or gonorrhea, which typically show symptoms and are easily treated, come to mind. But with HPV, the infection often doesn’t cause any noticeable symptoms until cell changes occur in the cervix. Some of the symptoms to watch out for include unusual vaginal bleeding or discharge, or pain and discomfort during sex (3).
Many people do not seem to know that HPV and cervical cancer are linked. Why is that?
Danielle: This lack of awareness is largely due to a misunderstanding of what HPV is and how it leads to cervical cancer. Many people don’t realize that cervical cancer screening is not just about checking for abnormal cells, but also about identifying high-risk HPV types that can cause changes in cervical cells. Since HPV doesn’t always cause symptoms, it’s easy to overlook the connection between the virus and the risk of cancer.
Another reason is that the focus has historically been on Pap tests, which look for abnormal cells, not the HPV itself. Currently, HPV primary screening, which tests for the virus directly, is recommended. This allows for earlier intervention and is more effective at preventing cervical cancer (4). The shift to HPV testing as primary screening in many countries has been a major step forward in the fight against cervical cancer.
Poll data shows that half of women in the U.S. don’t know how often they should get screened for cervical cancer (5). This lack of awareness is made worse by gaps in sexual health education and public health messaging. In the United States, sexual and reproductive health education often falls short, which likely contributes to the disconnect and stigma surrounding HPV and cervical cancer screening. Many people see Pap tests as something they “just need to do,” without fully understanding the purpose or what it’s testing for. But as HPV screening becomes more common and education improves, we can close these gaps and reduce the risks of cervical cancer.
What are the benefits of HPV testing for primary screening?
Danielle: HPV primary screening focuses on the root cause of cervical cancer: the virus itself. This shift allows for earlier detection and more effective prevention. One of the biggest benefits is that it also makes self-collection tests possible. In many countries, including the Netherlands, Denmark, Sweden, Australia, and Canada, self-collection tests are already part of their national HPV screening programs (6,7). In the U.S., two companies now have FDA-approved self-collection tests available, but only for use in healthcare settings (8).
Self-collection allows individuals to collect their own sample during a healthcare visit instead of undergoing traditional cervical screening with a speculum. This is particularly important because many people have personal or physical reasons for avoiding or delaying pelvic exams. In the U.S., a large number of women have delayed a Pap test because of fear or discomfort (5). Until now, there hasn’t been a good alternative for them.
HPV primary testing is recommended by major health organizations, including the World Health Organization (WHO), the American Cancer Society, the American Society for Colposcopy and Cervical Pathology (ASCCP), and experts at the National Institutes of Health (NIH) because it is more effective for cervical cancer prevention compared to Pap tests (9-12). However, in the U.S., adoption of this method has been slow, despite its effectiveness (4). It’s time for healthcare providers to embrace HPV primary testing as the best way to prevent cervical cancer.
What makes self-collection tests so appealing for people who feel anxious or uncomfortable with traditional in-office pelvic exams?
Danielle: Self-collection tests are appealing to many people because they offer more privacy, which can help reduce anxiety and make the process feel less intimidating for those who may find pelvic exams uncomfortable. Many people don’t need a full pelvic exam if they don’t have symptoms. With self-collection, you can collect your own sample during a healthcare visit without needing the full pelvic exam, stirrups, or speculum. This can help some people feel more at ease and less vulnerable.
For those who have had bad experiences with a pelvic exam, have conditions that cause discomfort, have experienced sexual trauma, or are transgender or gender diverse, self-collection can be a huge step toward feeling empowered. We also know that transgender people are nearly four times more likely to go unscreened than cisgender women (13). Self-collection helps remove some of those barriers and gives everyone a chance to take control of their health.
Can you walk us through how self-collection HPV tests work and how they differ from the traditional screening tests performed by a clinician?
Danielle: A self-collection HPV test is a simple swab that a person with a cervix can use to collect their own vaginal sample, either in a healthcare setting or, in some countries, at home. The process is straightforward: you insert the swab into the vagina, rotate it for 10-30 seconds, place it back into a tube, and hand it over to your healthcare provider to send to the lab. This is an easy, non-invasive method that gives individuals more control over their health.
The main difference with a clinician-collected HPV test is that the sample is taken directly from the cervix using a speculum. Sometimes this is done at the same time as a Pap test (when these tests are performed together, it’s called co-testing). However, we know that HPV sheds in the vaginal area, which is why self-collection from the vagina is just as accurate as a clinician-collected sample in detecting the virus (12). Plus, it can be more comfortable for people who might feel nervous or have difficulty tolerating a speculum exam.
Self-collection could also be done before a scheduled appointment, so the results are ready to discuss with your healthcare provider right away. This not only provides clarity on the next steps, potentially reducing fear and making the process more manageable, but it also creates an opportunity to have an open conversation about sexual health and gain information in the process.
How can self-collection HPV tests help people who have reduced access to traditional screenings?
Danielle: Self-collection tests can help reach underserved communities that are hit hardest by cervical cancer. This includes people with disabilities, those living in rural areas, or anyone facing logistical challenges in accessing care. In the U.S., more than half of cervical cancer cases happen in people who have never been screened (13). Self-collection HPV tests can help bring screenings to these communities, particularly through mobile health units that can deliver the tests directly to people. This makes it easier for people to get screened regularly, even if they have limited access to traditional healthcare settings.
Self-collection tests also have the potential to reach people who didn’t even know they needed screening. For example, if someone goes to a primary care appointment for diabetes or high blood pressure, or even for an unrelated urgent care visit, we can offer self-collection as an option if a pelvic exam isn’t feasible. This approach helps us engage patients in screening who may have never been screened or who might have fallen through the cracks. We know that 1 in 10 Black and Hispanic women have never had a Pap test or OB/GYN visit, and mortality rates are twice as high in high-poverty areas compared to low-poverty areas (14,15). Self-collection is a great way to reach more people and help close that gap.
What about self-collection in the home? When might this be available in the USA?
Danielle: Right now, in the U.S. self-collection tests are only FDA-approved for use in healthcare settings. But we’re seeing great results from countries like Sweden, where self-collection is already available at home. Sweden has had so much success with this approach that they’re on track to eliminate cervical cancer as a public health concern within the next five years (16). Eventually, self-collection at home will be available in the U.S. as well, making it even more accessible. This is a big step toward universal access to HPV screening, especially for people who face barriers to getting screened in a clinic.
What are some common misconceptions about self-collection HPV tests?
Danielle: One common misconception, even among healthcare providers, is that self-collection isn’t as accurate as having a clinician collect the sample. However, studies show that self-collection is just as reliable when done correctly (17,18). In fact, we know from large-scale modeling studies that increasing screening rates is more effective in reducing cervical cancer in the U.S. than increasing vaccination rates (19). So, having more options for screening, like self-collection tests, is key.
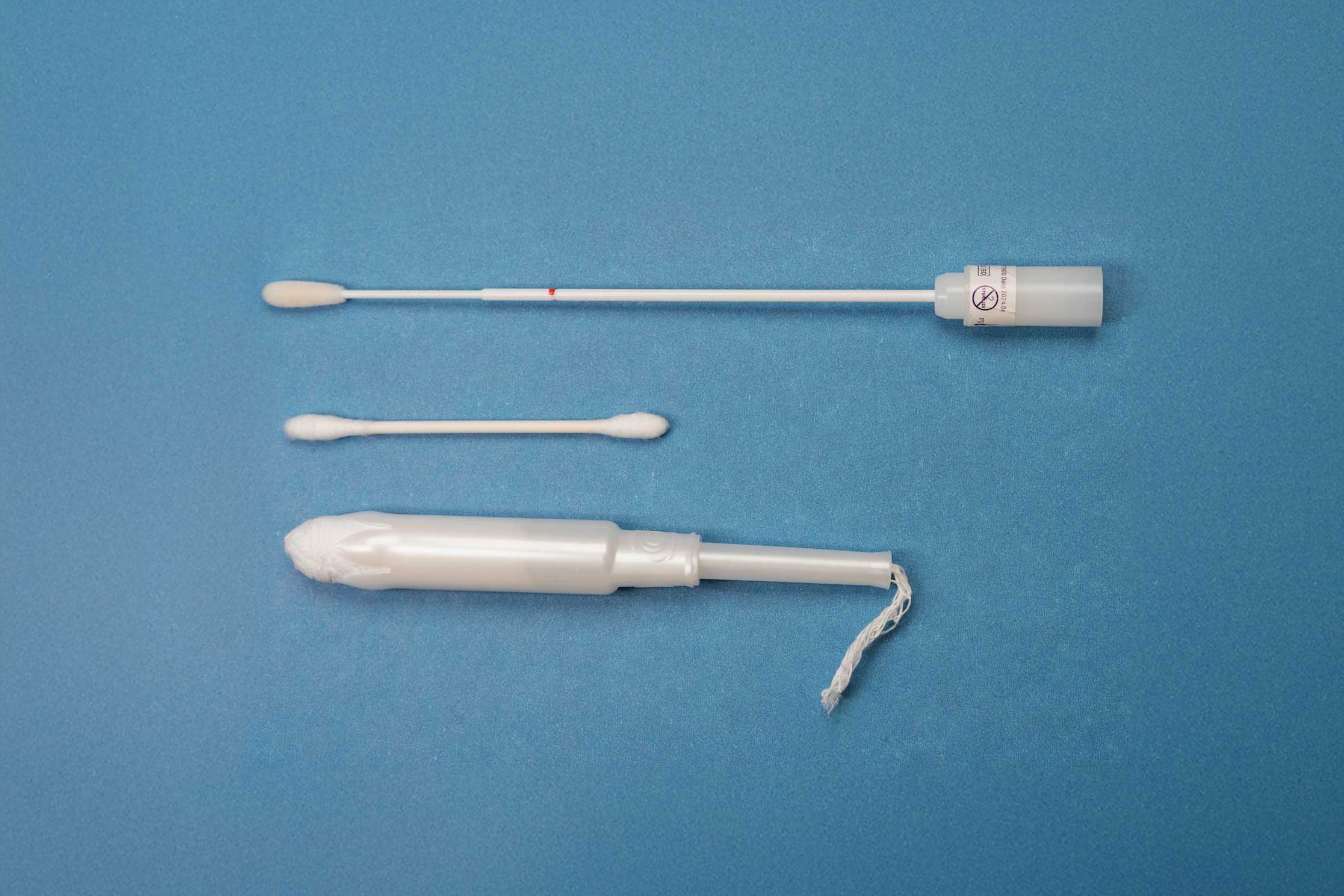
Another misconception is that people need special training to collect the sample, but that’s not the case. The process is simple and doesn’t require any special skills. The swab itself (which looks similar to a COVID swab) is small and less intrusive than a tampon or speculum, which makes it a lot less intimidating for many people.
How can Clue or other health apps support individuals through the screening process?
Danielle: Apps like Clue can be really helpful in reducing the stigma around HPV and guiding people through the screening process. Clue offers educational content about HPV and cervical cancer, helping people understand why screening is so important. With in-app features like custom tags and appointment tracking, people can track their screenings and test results, keeping all their health information organized and in one place. By offering education and easy ways to track screening, Clue helps people stay on top of their health and take proactive steps toward prevention.
What should someone do if they’re unsure where to start with HPV screening?
Danielle: If you’re unsure where to start, talk to your healthcare provider. Whether it’s your primary care provider or a gynecologist, they can help you figure out when to start screening and how often to do it. If you don’t have a provider, there are clinics and community health centers that can help. Guidelines can vary depending on where you are, so it’s an important conversation to have. If you’re interested in self-collection, ask if it’s an option at your clinic, and make sure you’re comfortable with the screening method. The most important thing is to start the conversation and take that first step toward prevention.
What would be your message to anyone hesitant about getting screened?
Danielle: I am on a mission to empower women and all people with a cervix to protect themselves from cervical cancer. This disease is preventable through vaccination, regular screening, and timely treatment. Screening is the best way to catch high-risk HPV types early, and early detection can prevent cancer. Don't let fear or uncertainty hold you back—getting screened is a simple but powerful step toward taking care of your health. Together we can eliminate cervical cancer!
Conclusion
HPV screening is key to preventing cervical cancer, whether done by a healthcare provider or through self-collection. Self-collection tests are making screening more accessible and comfortable for many people. Whether it’s due to fear, discomfort, or lack of access to care, self-collection HPV tests provide a simple and empowering way to take control of your health. By staying informed through resources like Clue and getting regularly screened, you’re helping to reduce cervical cancer rates and improve public health.
