Illustration: Marta Pucci
What are postpartum mood disorders?
How pregnancy and birth can impact your mental health.

You’ve probably heard of postpartum depression—it affects about 1 in 5 birthing parents and is a leading cause of maternal death (1-4). There isn’t a ton of research on postpartum depression, but researchers are beginning to understand more about the disease and its causes. Alongside postpartum depression, birthing parents can experience a variety of mood disorders. Raising awareness of postpartum mood and anxiety disorders can encourage birthing parents to seek help and reduce feelings of isolation.
When do people develop postpartum mood disorders?
While it is possible to develop a mood disorder immediately after birth, symptoms can emerge any time within the first 12 postpartum months (5). For some people, mood disorders first appear during pregnancy and then worsen postpartum (6). It’s also possible for non birth parents to experience postpartum mood disorders (6), but in this article we are going to explore postpartum mood and anxiety disorders as they apply to birthing parents.
If you ask someone who experienced postpartum depression, they are likely to tell you that their experience went beyond depression. Conditions like anxiety, obsessive compulsive disorder (OCD), posttraumatic stress disorder (PTSD), and psychosis can be just as debilitating as postpartum depression, or constitute a mental health emergency. Most people who are diagnosed with postpartum depression also experience another mood disorder, although it is possible to have another postpartum mood disorder and not experience depression (7).
Friends, family, and healthcare providers often overlook or diminish the suffering of a person with a postpartum mood disorder (5, 8). The symptoms of these conditions like fatigue and changes in appetite are also associated with caring for a newborn and can be brushed off (5). People with postpartum mood disorders often face barriers to being diagnosed and receiving treatment (8). Even when symptoms are obvious, clinicians are ill-prepared to diagnose and treat postpartum mood disorders (5, 8). There are no official diagnostic codes for postpartum mood disorders (DSM) and screening tools specifically for postpartum mood disorders other than depression don’t exist (8). When a postpartum mood disorder is diagnosed, it can be difficult and expensive to find treatment, and there’s no one-size-fits-all treatment that can guarantee a cure (8). While pregnancy and birth can be life threatening, particularly for people of color in the United States of America who are more at risk for adverse maternal health outcomes due to systemic racism, the same racial and ethnic health disparities make resources even less available for Black and Latina women in the USA suffering from postpartum mood disorders (9).
What causes postpartum depression and other postpartum mood disorders?
No specific cause of postpartum mood disorders has been determined yet, but there are a few theories. The sex hormones estrogen and progesterone fluctuate wildly during the transition from pregnancy to postpartum (6). Researchers believe that these hormones may play a role in postpartum mood disorders (6).
Another theory involves neurotransmitters, your body’s chemicals that send messages to nerve cells. (You may have heard of serotonin or dopamine, two “feel good” neurotransmitters.) Hormones and neurotransmitters work together in the body, potentially contributing to mood changes during reproductive events like birth (4).
Some other potential causes under investigation include genetic predisposition, melatonin levels, thyroid function changes, and immune system responses (4). We don’t know for sure why a person experiences one mood disorder and not another.
Types of postpartum mood disorders
It’s more than just depression. Let’s take a look at some of the postpartum mood disorders that are currently recognized.
What are the baby blues?
The baby blues, also called the postpartum blues, are a common reaction to bodily changes that take place after birth (6). The pregnancy hormones estrogen and progesterone are high during pregnancy, but dip dramatically after birth (6). The result may be sadness, insomnia, irritability, anxiety, and tearfulness (6). The baby blues are common right after birth, may peak around day five postpartum (6), and may last for up to three weeks (6). Research suggests up to 75% of postpartum people experience the baby blues (6).
What is postpartum depression?
Peripartum depression, or depression that occurs during pregnancy or postpartum, is believed to be the most common mood disorder in pregnant and postpartum people (5). Estimates of postpartum depression are hard to determine. Research indicates postpartum depression affects 10-15% of postpartum people (10), but the number is likely much higher. Studies of postpartum depression often only include the first few weeks postpartum, when postpartum depression may occur any time within the first postpartum year (10).
People experiencing postpartum depression may experience trouble sleeping or oversleeping, depressed mood, loss of interest in activities, weight loss, restlessness or slow movements, fatigue, and/or feelings of worthlessness or guilt (6). Some science indicates that loss of control is the predominant feeling throughout postpartum depression (6). Postpartum parents with depression often feel as though they are struggling to survive, enveloped in fogginess that makes it difficult to focus on even simple tasks including caring for their infant (6).
What is postpartum anxiety?
Postpartum anxiety is an umbrella term for a group of anxiety disorders that includes generalised anxiety, panic, and social anxiety disorders (10). It’s hard to determine how many people experience postpartum anxiety, but it’s likely that depression and anxiety disorders impact postpartum people equally (10). Most people who experience postpartum depression will also experience clinical levels of anxiety (10).
It’s normal to worry about your fetus or newborn, but postpartum generalized anxiety disorder (GAD) occurs when worry becomes excessive and uncontrollable and interferes with daily life or taking care of an infant (8). Worries might cover a broad spectrum, but it’s common for people with postpartum anxiety to worry about the health of their newborn, their own health, the health of their partner, and/or dying and leaving the newborn without a parent (8).
A person who has sudden, unexpected panic attacks after birth of an infant may have postpartum panic disorder (11). This form of postpartum anxiety can be diagnosed when the attacks continue for over a month and the person is persistently worried about having another attack (11). Postpartum panic disorder might make someone feel like they’re losing control, going crazy, or even having a heart attack (11).
There isn’t currently much research specifically on postpartum social anxiety, but one study found that people who were not breastfeeding their infants were more likely to have postpartum social phobias (12). Social anxiety is associated with extreme fear of social judgment and avoidance of unknown people (12). People with postpartum social anxiety are more likely to report relationship problems during the postpartum period (12).
What is postpartum OCD?
Postpartum obsessions can vary, but many people with postpartum OCD say that it centers on thoughts about harming their infant (13). Other common obsessions are cleanliness or checking things (13). It’s important to note that people with these obsessions are not likely to hurt their infant and it’s likely that the obsessions are unwanted and not consistent with the person’s true thoughts or character (13).
Obsessions aren’t just strong preoccupations with certain things. Psychologically, an obsession is a recurrent and persistent thought that causes anxiety or stress (13). The thought might manifest as an image that the person with OCD can’t get out of their head (13). The thoughts and images are often offensive or inappropriate and unwanted (13). A person with OCD may have an impulse to perform a behavior that relieves them of the thought or image—this is the compulsion part of OCD (12). Some data suggests about 9% of people experience postpartum OCD after birth and of these, almost 40% also have depression (13).
What is postpartum PTSD?
Although PTSD was first identified in soldiers who served during war time, it is also a common experience following pregnancy and birth (14). PTSD onset can occur when a person experiences an event during which they feel their life or safety is threatened (14). A person with PTSD might feel like they are re-experiencing the event and avoid people or places that remind them of the event (14).
People who experience a traumatic pregnancy or birth are at risk for postpartum PTSD (14). A person with postpartum PTSD may decide not to have more children, delay having more children, or choose a cesarean section during their next birth because of their traumatic experience (14). It is common for a person with postpartum PTSD to also experience postpartum depression (14).
What is postpartum bipolar II?
Bipolar II is often called “the postpartum depression imposter” because people with undiagnosed bipolar II may see their symptoms peak postpartum and seek treatment (6). Sometimes people with bipolar II may try different treatments for postpartum depression that are all unsuccessful (6).
The symptoms of bipolar II often look a lot like postpartum depression. People with this condition may experience days-long bursts of energy immediately after birth, but settle into severe depression after a few weeks (6). People with postpartum bipolar II describe it as intense depression with occasional sudden, intense bursts of emotional energy that feel like they were flipped on by a switch (6).
What is postpartum psychosis?
Postpartum psychosis is considered the most severe postpartum mood disorder because both suicide and infanticide are risks of the disease (6). Most people who experience it will begin to show symptoms a few days to three weeks after birth (6). Friends or family may notice it’s hard to communicate with the person with psychosis (6). They may be out of touch with reality, having rapid mood swings, or hallucinating (6). They may have noticeable changes in appetite or sleep (6). If you think you or someone you know is experiencing postpartum psychosis, call a healthcare provider or the emergency services immediately, because it is considered a medical emergency.
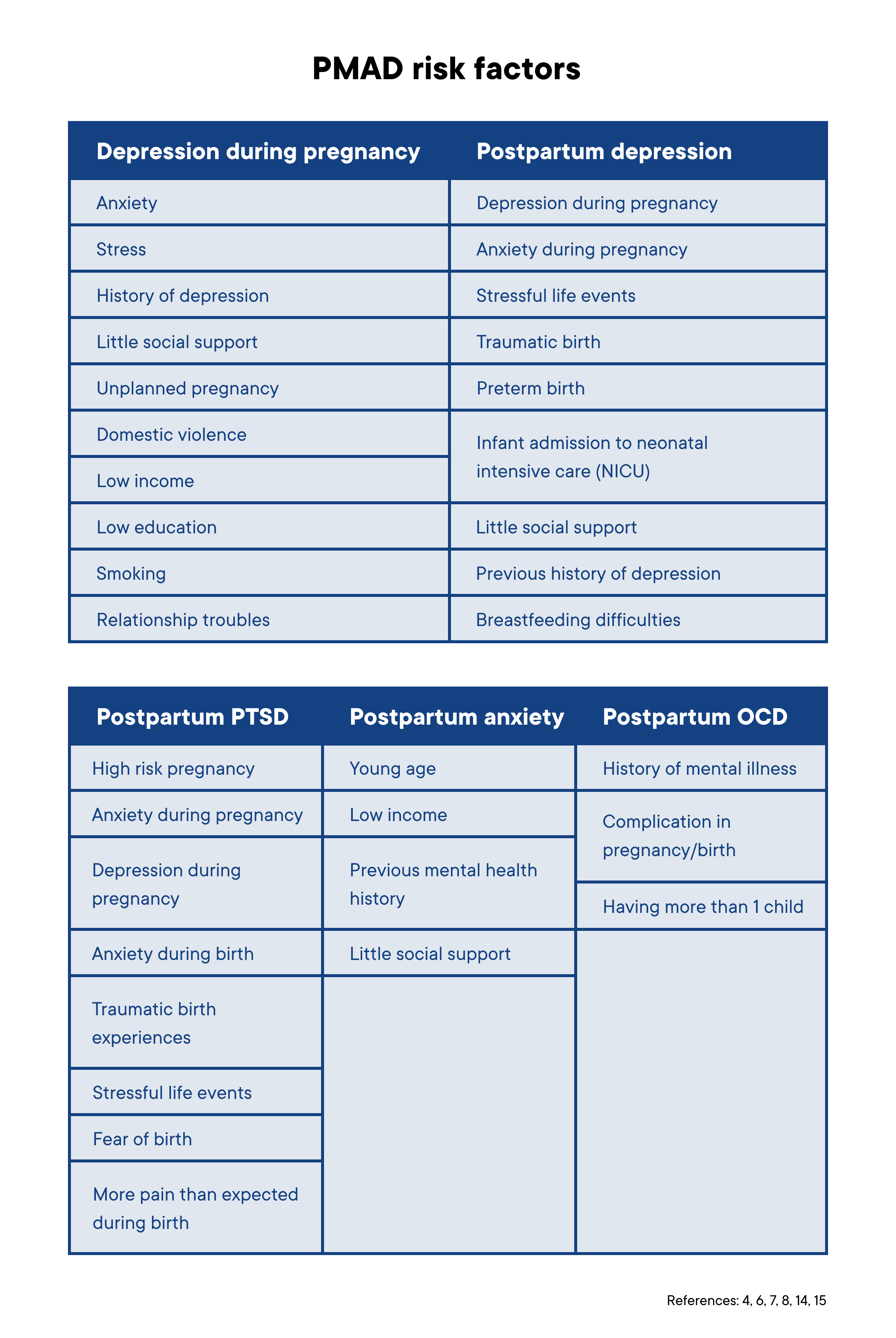
Who is at risk for postpartum depression and other mood disorders?
The risk factors for pregnancy and postpartum mood disorders vary depending upon the condition. Overall, a history of previous mental illness may be the strongest indicator of risk for a postpartum mood disorder (5).
Getting help for postpartum mood disorders
The time following the birth of a newborn is sometimes called “the fourth trimester” (16). Cultural norms surrounding this time are likely to influence rates of postpartum mood disorders (6). Lack of time off from work, social isolation, and lack of postpartum rituals may all contribute to the development of these conditions (6). Some research shows that educating new parents about expected postpartum changes and newborn behaviors can reduce the risk of postpartum mood disorders (17), but these programs can be hard to come by.
If you are living with a postpartum mood disorder, know you are not alone and it’s not your fault. If you feel shame or embarrassment, know this is normal and your symptoms do NOT make you a bad parent. There are well-researched treatments for the symptoms of postpartum mood disorders, including medication and therapy (17). There is no cure yet, but medications can improve quality of life. Talk to your healthcare provider about which medications or therapies might be right for you. There are several medications that are safe to take if you are breastfeeding/chest feeding (18). If you can’t leave the house, consider trying a telemedicine platform like Maven that has specialized providers who can see you at home.
If you or someone you love is experiencing a postpartum mood disorder and not getting the medical care or community support you need, Postpartum Support International can help you find resources in your area. In the USA, you can call them at 1-800-944-4773. If you are having thoughts of hurting yourself or your infant, or feelings that your infant would be better off without you, please seek medical help immediately.
Download Clue to track your pregnancy and mental health.
