


A podcast about how hormones shape our world.
Latest episode:
Who you gonna call? Mythbusters!
About Hormonal
Hormones affect everyone and everything: from skin to stress to sports.
But for most of us, they're still a mystery.
Even the way we talk about hormones makes no sense. ("She's hormonal.")
So let's clear some things up. Each week, Rhea Ramjohn is asking scientists, doctors, and experts to break it all down for us.
Subscribe on your favorite platform:
Episodes
- Season 1
- Season 2

Episode 0
August 25, 2020
A Sneak Peek at Season 2
As we work hard on Season 2 of the Hormonal podcast, we’re dropping into your feed with a special request, and a small behind the...
5 min

Episode 1
October 11, 2020
Hot or not? Birth control & sex drive
How birth control affects your sexual desire, self image, and weight fluctuations.
25 min
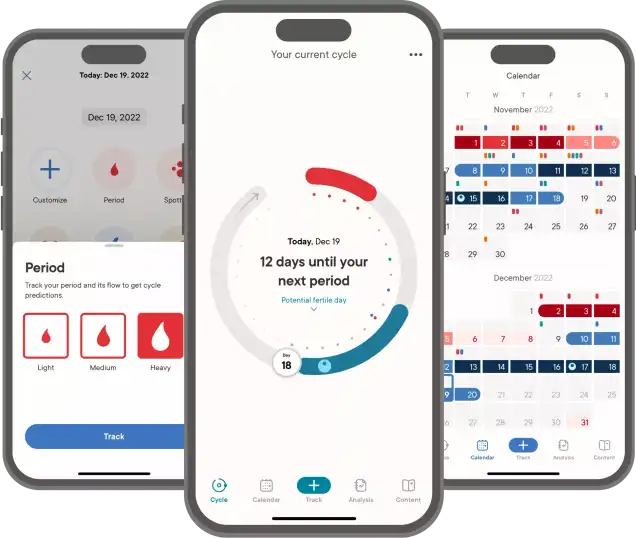
Support Hormonal & the period tracker that’s different from the rest.
Subscribe to Clue Plus
Episode 2
October 19, 2020
The ABC: Abortion & Birth Control
What’s it like to get an abortion and the surprising ways the pandemic is changing abortion access.
34 min

Episode 3
October 26, 2020
The many sides of side effects
Hormonal birth control: positive, negative, and neutral effects
33 min
Support Hormonal & the period tracker that’s different from the rest.
Subscribe to Clue Plus
Reproductive choice and reproductive justice
with Dr. Loretta Ross
Episode 4
November 2, 2020
Reproductive choice and reproductive justice
Accessing birth control against the odds
35 min

Episode 5
November 9, 2020
Happy birthday, birth control
Controversy and celebration on the 60th anniversary of the pill
42 min


Episode 7
November 23, 2020
Risky business: birth control during COVID-19
COVID-19 is changing how we access birth control
30 min
Support Hormonal & the period tracker that’s different from the rest.
Subscribe to Clue Plus
Who you gonna call? Mythbusters!
with Lynae Brayboy, Amanda Shea & Hajnalka Hejja
Episode 8
November 30, 2020
Who you gonna call? Mythbusters!
Clue’s Science Team busts your birth control myths
37 min
Credits
Season 2
Executive Producer: Kassandra Sundt
Host: Rhea Ramjohn
Editorial Help from: Amanda Shea, Steph Liao, Nicole Leeds
Clue Design: Marta Pucci & B.J. Scheckenbach
Web Team: Yomi Eluwande, Jane Parr-Burman, Maddie Sheesley
Special Thanks: Trudie Carter, Ryan Duncan, Aubrey Bryan,
Claudia Taylor, Léna Calvarin, Lynae Brayboy
Mixing and recording help from: Bose Park Productions & Rekorder Studios in Berlin.
About Clue
Clue is a period tracking app that uses data and science to help women and people wih cycles to understand their bodies. It's also a menstrual and reproductive health encyclopedia.
Learn more about the Clue app and check out what Clue is doing to advance menstrual health research.


Rhea Ramjohn,
host of the Hormonal Podcast


Rhea Ramjohn,
host of the Hormonal Podcast
Your Host
The more knowledge we have about our hormones, our medical & menstrual care, and our reproductive rights, the more we empower ourselves and one another.
Hormonal has offered me the true privilege of speaking with people who have the expertise on the scientific knowledge about our hormones and cycles, as well as those sharing their lived experiences, caring for people with menstruation and how, all combined, shapes our lives everyday.
Gathering facts as well as personal stories are so vital to our understanding of our health, our his/herstories, and our cultures. I deem it a privilege because we haven't had many platforms nor opportunities for menstrual health information being broadly accessible.
Episode 7
Risky business: birth control during COVID-19
Risky business: birth control during COVID-19
COVID-19 is changing how we access birth control
About
The COVID-19 pandemic has upended healthcare systems around the world, especially reproductive healthcare. Gillian Sealy of the US nonprofit “Power to Decide” joins us to discuss how the pandemic has influenced birth control access.
Transcript
This transcript and interview were edited for clarity.
On Hormonal we explore the science behind hormones. But we also talk about society and the world around us. On Hormonal, we know that there are lots of women who have periods and lots who don’t. We also know that there are people who aren’t women who have periods too. We also know we have listeners who have never had periods. We hope you feel welcome, even when a term that a guest uses maybe doesn’t apply to you.
At Clue, we believe that our identities are not determined by our bodies. Thanks for listening to Hormonal.
Rhea Ramjohn: Hi, I'm Rhea Ramjohn, and you're listening to Hormonal, brought to you by Clue, the menstrual health app.
This season has been all about birth control, but in the background of a lot of our episodes has been, well, a worldwide pandemic.
It's upended foundations, institutions, and services that we thought were stable and may have taken for granted, like the airline industry, for instance. And it's put many of us into precarious and even more vulnerable positions.
Think of our essential workers, artists and freelancers, and really all of us.�
So bringing it back to our birth control theme for this whole season, we wanted to know - how is covid-19 impacting birth control and reproductive rights? How is access changing or possibly innovating?
We're joined today by Gillian Sealy. She's the interim CEO of Power to Decide. They're a nonprofit in the U.S. focused on preventing unplanned pregnancy and helping young people find a birth control that works for them. She joins us today from Tampa Bay, Florida. Gillian, welcome.
Gillian Sealy: Good morning. Thank you for having me. I'm looking forward to this discussion.
Rhea Ramjohn: So, Gillian, before we talk about the “Thanks Birth Control Study” that your organization recently conducted, can you tell us who is most vulnerable to losing access to birth control and reproductive care right now?
Gillian Sealy: I think really and truly, we really need to understand what's at stake as it relates to reproductive health and sexual health and access to contraception. We do know that there was a vacancy on the Supreme Court, but I think it's much more than that. We also want to make sure as we look at policies that will be happening within the next few weeks and months around access to insurance, right? Because we know that having insurance allows people, in this particular case, young people and women, to be able to use their insurance care to access contraception. In addition, we want to make sure that at the federal and state level, there are policies that are supportive of reproductive health and sexual health, including contraceptive access and abortion.
Rhea Ramjohn: So we’re talking to you today because your organization, Power to Decide, did your annual Thanks Birth Control Survey. How have this year’s survey results compared to previous years? How has the pandemic affected birth control users?
Gillian Sealy: What we have seen and, you know, we did the Thanks Birth Control Survey about the impacts of COVID-19 and 80% of those polled, and these were birth control users 18 to 34, said that birth control has allowed them or their partner to worry about one less thing during the COVID pandemic. And 8% of those respondents said that they or their partner planned to get pregnant in the next 12 months. So the fact that 8% of respondents said that they or their partner planned to get pregnant in the next 12 months, suggests that there is a possibility that, you know, people are looking at LARCs and other forms of birth control to delay pregnancy over the long-term, especially as this pandemic continues to to rage on and we don't know when the pandemic will be over. So I think people are making plans for their lives around delaying pregnancy, delaying having a family and really thinking a lot more about their reproductive and sexual health lives during this pandemic.
Rhea Ramjohn: In the intro, I mentioned the vulnerability and instabilities that the pandemic has further exposed. So prior to the pandemic, how secure was birth control access in the U.S.?
Gillian Sealy: So pre-COVID, we were very concerned about access to contraception. For instance, women have always faced barriers when it comes to accessing contraception; whether those are financial barriers, lack of insurance, transportation, being unable to access child care, and these are just a few of the barriers that we know that women face. This is particularly hard for marginalized populations, women in poverty, women of color, women living in rural areas. So these were the things that we saw and we were acutely aware of pre-COVID. The pandemic has just exacerbated the lack of access for those people in particular. And Power to Decide has always been and continues to be concerned with how to make sure that people are still accessing the contraception in the middle of a pandemic, and what resources are the best for them so that they can get what they need.
Rhea Ramjohn: Mm-hmm. Obviously, security and vulnerability vary all over the world. So what's the frame that our worldwide listeners can think about when considering birth control access? For example, I would imagine that living in a country with universal health coverage would make access more secure, or am I wrong to assume that?
Gillian Sealy: The pandemic is global, right? The fact that it is considered a pandemic means that it's global. So regardless of where you are, with stay-at-home orders, closures of university health centers, concerns of being exposed to the virus, getting to a clinic to be able to access birth control has become even harder, especially for young people. When you couple that with widespread job loss due to COVID-19, which has left thousands of young people without health insurance or the necessary income to purchase contraception. It really has changed our approach to healthcare, and especially for women trying to avoid an unplanned pregnancy. Wanting to make sure that you have access to contraception is something that is top of mind for many of them and their partners.
Rhea Ramjohn: I just wanted to ask and follow up there— you mention young people specifically, is that because of job or economic insecurity, or the university closures like you just mentioned? Break that down for us.
Gillian Sealy: I think it's more than the economic factor. I think, you know, just having access again, being able to have face-to-face visits with your healthcare provider has just been very, very hard to come by, especially in places where you have safer-at-home or stay-at-home orders. So that has really made the barriers even harder for young people. And in fact, it has had young people really thinking about their reproductive health. For instance, whether they will delay having a child or having a pregnancy because of the access issues.
Rhea Ramjohn: So as the pandemic started to unfold, what were the concerns that Power to Decide, which is your organization, had?
Gillian Sealy: I think there were a few of them. We talked about the access issues, right, about folks being able to go in and get their birth control. But we also saw, for instance, since March, there were quite a few states who were using the pandemic to further restrict abortion access. We placed our efforts in informing people that abortion is legal in the United States and where they can access the full range of reproductive health services and methods in the pandemic with restrictions. So, for instance, there were eight states, Louisiana, Texas, Oklahoma, Tennessee, Alabama, Iowa, Ohio, and Arkansas, that use the COVID-19 pandemic as an excuse to ban abortion by deeming it a non-essential procedure. And as we know, abortion is indeed extremely time sensitive, especially in states with waiting periods and few providers. And while since March, most of these bans have expired or were defeated by legal challenges, we do know that abortion care continues to be under attack. And I can't reiterate that enough, abortion and abortion care is time sensitive, especially for women of low income, women who have to travel outside of their state to access abortion care. So these are some of the things from a policy perspective that we're very concerned about in addition to access in terms of transportation, child care, financial barriers, etc.
Rhea Ramjohn: Of course. So can you describe concretely for me how the pandemic has actually changed access to all those services you've just described?
Gillian Sealy: Absolutely. So as I mentioned, in terms of the pandemic: not having access to your provider, the closure of university health centers, people worrying about being exposed to the pandemic, widespread job loss. We did a poll and 80% of polled birth control users, 18 to 34, said that birth control allowed them and their partners to worry about one less thing during the pandemic. So if they don't have access to birth control, this is one more thing, in addition to all the things that I mentioned that are barriers that they have to worry about.
Rhea Ramjohn: Yes.
Gillian Sealy: You know, and as I mentioned, COVID-19 has really changed our approach to healthcare for women trying to avoid an unplanned pregnancy, including how to access contraception. And what we have seen is, for instance, that telehealth is really a viable option as it relates to providing access.
Rhea Ramjohn: You’ve mentioned Telehealth, which is kind of a catchall term that includes lots of different new and innovative ways of using electronic platforms, apps and video calls and the like to provide medical care as opposed to face to face meetings with a doctor or health care provider. So, Gillian, do you see telehealth as filling a gap?
Gillian Sealy: We do see telehealth as filling a gap, but I want to be careful here and point out that everyone doesn't have access to telehealth services, right? We do know that there are those who don't have stable Internet connections and so cannot access telehealth and we recognize that barrier. However, we do see telehealth as a viable option. It's gaining tremendous support not just among patients, but also among care providers. And it really is important to understand that the convenience and effectiveness of telehealth, again, are a viable option. But I would want to put a pin here to say that in addition to those not having stable Internet access to access telehealth, it's really important to understand that the effectiveness of telehealth can be, and is, experienced disproportionately among women with higher incomes. So, for instance, a recent survey that was released by Power to Decide shows that significantly more respondents with an annual household income of $50,000 or more understood what telehealth was; 69% of them reported being able to use telehealth and then 68% of them knew how to find a telehealth provider compared to women with household incomes under $50,000, right. And so for women with lower incomes, and that means those under fifty thousand, only 21% knew or understood what telehealth was. So I want to be very clear that while telehealth is a viable option, there's still many disparities that we're seeing around this issue.
Rhea Ramjohn: Yeah, that's very disconcerting. It's just another example of how this pandemic is exposing so many vulnerabilities that were already there before the pandemic. So can you explain that gap? Like what is the reason for that gap?
Gillian Sealy: I think there are many reasons for the gap. We have to be very clear that the pandemic just has exposed many of the barriers to contraception that we have seen pre-COVID, right. I think, you know, COVID has just shined a light on what a lot of these access issues were. In addition to the ones that I just mentioned, supportive policies that support birth control and contraceptive access, sexual and reproductive health are really a key to making sure that people have access. Another example would be [how] Medicaid coverage expansion allows access to health insurance coverage that can help more women access the most effective methods of contraception by again removing those cost barriers. And we know that Medicaid is a vital source of health coverage, including for contraception. However, 12 states still have not expanded Medicaid for low income adults as allowed for by the Affordable Care Act. So in addition to those barriers that I mentioned, they are barriers from the political standpoint that also make it very difficult for people to access contraception, and I think that we're mindful that some of this might happen post-COVID as well.
Rhea Ramjohn: Telehealth is just one of those things that’s so interesting, because it has the potential to really change, in an on-the-ground way, how people access care. And I don't want to stay on this topic for too long, because I do have a lot of questions about your study as well, but I have two really important follow up questions about this.
Do you think that doctors are making information about telehealth services available to patients and prospective patients? And also, what about pharmacist-prescribed birth control?
Gillian Sealy: Yes, so I think that both providers and patients see that telehealth is important, especially during this pandemic, to be able to access contraception. Definitely there is a need for additional information, and so Bedsider, which is our online birth control support network, where we provide resident information on all methods of birth control so that people can find a method that works best for them, especially during this time. We have been doing lots of work to provide information, not just to the patients, but also to care providers on telehealth and the best ways to be able to access it and the importance of it. So more information and education is clearly needed for both parties. And I will say that post-COVID, there is the possibility that patients and providers will want to see telehealth expanded to be able to serve their patients and allow for, again, greater access.
In terms of pharmacists prescribing, policies at the state level could make it harder or easier to access birth control over the counter. So, for example, currently there are 17 states, including the District of Columbia, that have enacted policies to allow pharmacists to prescribe and dispense self-administered hormonal methods. So that would include the pill, the patch, the ring, the shot. And so given this landscape, and ongoing federal policy challenges, interest in allowing pharmacists to prescribe hormonal contraception is likely to continue to gain traction in these states. In fact, new research from Oregon, California, Colorado, and Hawaii suggests that this model is helping to fill a gap.
Rhea Ramjohn: Gillian, we have a lot more to discuss about how this pandemic is affecting people’s access to reproductive care and birth control, but before we continue, let’s take a quick break.
Hormonal is brought to you by Clue: the period tracking app and menstrual health encyclopedia that takes your cycle seriously.
Clue has been around since 2012, and since then our community has grown to millions of people. And we want to be around for years to come.
But to do that, we need support from people like you. By subscribing to Clue Plus, you’re supporting the work here at Clue. You’re also keeping the app free for others who maybe don't have the same resources or access as you. And you’re helping fund important menstrual health research around the world.
To learn more about becoming a Clue Plus subscriber, go to Clue.plus.
Alright, back to the show.
Rhea Ramjohn: Welcome back to Hormonal. I’m your host, Rhea Ramjohn.
Gillian, as we all know, many of us first-hand, job instability and unemployment have increased over the course of the pandemic. In the US alone, there are millions without a job, and that’s, for a lot of people, their connection to their health insurance.
What does this mean for people who use birth control and their options?
Gillian Sealy: The pandemic has had devastating effects, not just from a health perspective, but also from an economic perspective as well, and has caused people to lose their jobs, which has had an impact not just on their insurance, but also being able to afford their contraception out-of-pocket. So it has had devastating effects for them as well. And thinking about how they will be able to afford their contraception again, you know, it is time sensitive. You want to make sure that people continue their method of birth control and it's even more important during this pandemic, as they are not able to go to their doctors to be able to get their contraception. So, to your point, not being able to have insurance adds another layer of the barriers that people are seeing, being able to afford healthcare, but in particular their contraception as well.
Rhea Ramjohn: You alluded to this in the “Thanks birth control” survey that a lot of people aren't looking to have a baby in the next 12 months, and I think this kind of flies in the face of this joke at the beginning of the lockdowns earlier this year, that there would be these so-called, quote unquote, lockdown babies. It can be funny for some and not for others. So what is your reaction to these kinds of assumptions?
Gillian Sealy: I think exactly as you just said, they're assumptions, right? And just like you, I heard all those jokes and suggestions that we will probably see a boom in COVID babies. But I think that when you dig deeper and you look at the surveys that we at Power to Decide have conducted and released, and other surveys, people are really thinking about their reproductive and sexual health and what that means for their future–for a number of reasons. The reason why there was that assumption that there would be a baby boom is because people were going to be at home, they were sheltering in place. But more importantly, along with this pandemic has come all the other things that we talked about: economic barriers with people losing their jobs and losing their health insurance, and that having a devastating effect on their families and really having them think a lot more carefully about what that means to their family formation. So I think that's one of the pieces and one of the places where we will find out, you know, nine months, one year from now whether that assumption holds true. But I think it's just much more multifaceted than saying that people are at home so in nine months we'll see a baby boom. I think people are just carefully thinking about how this pandemic is affecting their lives, not just in the moment, but also for their future as well.
Rhea Ramjohn: What do you recommend to people trying to minimize trips to the doctor's offices or in public in general, but still want access to birth control? What are our best bets?
Gillian Sealy: I think there are a couple of things that you can do. First and foremost, I encourage people to go to Bedsider.org, which is powered by Power to Decide where we continue to update and provide resonant information about telehealth, not just what telehealth is, but how to access telehealth. And I would also encourage folks to talk to their healthcare provider. Even if you are accustomed to having an in-person appointment with your doctor or your healthcare provider, this is a prime opportunity to have a conversation with them as to whether telehealth is a viable option for you. I would also encourage people to reach out if they have health insurance to their health insurer to see if telehealth is something that is covered under their health insurance as well.
Rhea Ramjohn: What do you think providers have learned over the course of this pandemic about how they can better offer care? What have been the innovations?
Gillian Sealy: Based on the pandemic and based on the fact that we just have not been able to do face-to-face appointments and being able to see our healthcare providers, we've seen a boom in telehealth, and I want to be clear that telehealth was an option before the pandemic. But I don't think that there was the added need as well as desire for folks to use telehealth as a viable option, and healthcare providers are also seeing a viable way to reach patients, especially those who are most marginalized. So those who are living in rural areas, in areas of poverty, and especially for people of color, I think this is a really viable option to reach those patients who need access to care. And when I say access to care, I anticipate that this will obviously be a lot greater than just contraception. So this is probably going to be a new way that we see healthcare taking off post-pandemic. And even when you look at policies that might be being enacted now to allow for telehealth due to the pandemic, I think after the pandemic there's going to be a groundswell, especially from patients and likely healthcare providers as well for this to continue. So I think for healthcare providers, they really see this as a solution to a complex problem in terms of healthcare.
Rhea Ramjohn: You touched on this, but in general, are there changes that have come from the pandemic that you think are here to stay?
Gillian Sealy: The option of telehealth is something, in terms of whether we will see policies about how telehealth is enacted, that is something that we will see more of. It will be left to see, in terms of insurance companies, what their thinking is around telehealth and being able to offer that as a standard option for patients. Being able to use something like telehealth as a resource, for instance, to get birth control delivered to your door in a pandemic, is something that we will probably continue to see more of. As we talk about pharmacy prescribing, we will likely see, in addition to those 17 states, maybe other states who are also going to be thinking about that, because this goes much further than allowing for access during the pandemic, but allowing for access in general, especially for those for whom access has traditionally been and continues to be a major barrier.
Rhea Ramjohn: Mm-hmm. Gillian, 2020 has been hard to put into words. Let's just say it's been a tough year and it's likely that we won't see a resolution to the pandemic any time soon. So what is your big message to listeners who are worried about their own access, or access for others?
Gillian Sealy: There's no end in sight at this point, in terms of the pandemic, on what that looks like for millions of people across the world for access. Access was an issue for various populations before the pandemic, but this really shone a light, not just for individuals and the healthcare profession, but also policymakers and advocates, that we need to focus on access and what access looks like, and how we can make sure that all people have the access to the healthcare that they need, including for contraception and abortion care. COVID-19 has changed our approach at this point in time for how women, for instance, avoid an unplanned pregnancy, and this includes access to contraception. I will say that the pandemic has allowed us to look at telehealth as a viable option, [as well as] delivered-to-your-door contraception. And because we don't know when the pandemic will end, I suspect that we will continue to see these options and these topics being more focused on as we ride through this pandemic, but more importantly, after this pandemic is over, I suspect that we will continue to see calls for things like telehealth being more mainstream so that people have the access that they need.
Rhea Ramjohn: Gillian, we’ve talked a lot about the Thanks Birth Control Survey, and we have a link to that survey in the show notes. What jumped out to me is that there seems to be reasons for us to be optimistic. Could you expand on that for us?
Gillian Sealy: Absolutely, and in this survey, we specifically asked about the impacts of covid, and some of the top line things that we were able to glean from the survey is that 80% of polled birth control users, aged 18 to 34, said that birth control has allowed them and their partner to worry about one less thing during the covid pandemic, right, and as we talked about, there are many things to worry about during the covid pandemic. But this allows them to worry about one less thing. 82% of respondents, 18 to 34, said that they had access to accurate and reliable information about birth control, and we definitely know that this is really important because it allows people to get all the information that is resonant and accurate and then make an informed decision for themselves around their method of birth control.
Gillian Sealy: 94% percent of respondents, again, age 18 to 34 who use birth control, are actually thankful that birth control has allowed them or their partner to decide if or when to have a child. But again, we talked about during this pandemic how people are thinking about delaying having children or are thinking more about their reproductive and sexual lives. And so 94% of respondents were thankful for birth control that allows them to do this is a really good thing. And then 84% of respondents, 18 to 34, who use birth control are also thankful that birth control has allowed them or their partner the ability to work towards their professional and educational goals. So there is and are glimmers of hope during this pandemic. I would be remiss if I didn't also reveal one or two other things from the survey. So, for instance, 18% of respondents aged 18 to 34, reported that they were unable to see their provider for sexual and reproductive healthcare in person during the covid-19 pandemic. And this really highlights the importance of finding solutions for folks who are wanting to access contraception during this time and I go back to telehealth solutions, delivery to your door of hormonal contraception and others that make access much more viable during this time.
Rhea Ramjohn: Gillian Sealy is the interim CEO of Power to Decide, and she joined us from Tampa Bay, Florida. Gillian, thanks so much for making time for us today on Hormonal.
Gillian Sealy Thank you so much for having me.
Credits
Rhea Ramjohn: Hormonal is hosted by me, Rhea Ramjohn! Our Executive Producer is Kassandra Sundt.
Editorial help from:
Amanda Shea
Steph Liao
Nicole Leeds
Special thanks to:
Marta Pucci
Trudie Carter
Maddie Sheesley
Ryan Duncan
Aubrey Bryan
Claudia Taylor
Léna Calvarin
Lynae Brayboy
Yomi Eluwande
And Jane Parr-Burman
Mixing and recording help from Bose Park Productions and Rekorder Studios in Berlin.
Thanks for listening to Hormonal. Please rate and subscribe, and tell a friend! Until next time, I’m Rhea Ramjohn.
Related links:

Episode 7
November 23, 2020
Risky business: birth control during COVID-19
COVID-19 is changing how we access birth control
About
The COVID-19 pandemic has upended healthcare systems around the world, especially reproductive healthcare. Gillian Sealy of the US nonprofit “Power to Decide” joins us to discuss how the pandemic has influenced birth control access.
"In our recent survey, birth control users [ages] 18 to 34 said that birth control has allowed them or their partner to worry about one less thing during the COVID pandemic."
On Hormonal we explore the science behind hormones. But we also talk about society and the world around us. On Hormonal, we know that there are lots of women who have periods and lots who don’t. We also know that there are people who aren’t women who have periods too. We also know we have listeners who have never had periods. We hope you feel welcome, even when a term that a guest uses maybe doesn’t apply to you.
At Clue, we believe that our identities are not determined by our bodies. Thanks for listening to Hormonal.
Rhea Ramjohn: Hi, I'm Rhea Ramjohn, and you're listening to Hormonal, brought to you by Clue, the menstrual health app.
This season has been all about birth control, but in the background of a lot of our episodes has been, well, a worldwide pandemic.
It's upended foundations, institutions, and services that we thought were stable and may have taken for granted, like the airline industry, for instance. And it's put many of us into precarious and even more vulnerable positions.
Think of our essential workers, artists and freelancers, and really all of us.
So bringing it back to our birth control theme for this whole season, we wanted to know - how is covid-19 impacting birth control and reproductive rights? How is access changing or possibly innovating?
We're joined today by Gillian Sealy. She's the interim CEO of Power to Decide. They're a nonprofit in the U.S. focused on preventing unplanned pregnancy and helping young people find a birth control that works for them. She joins us today from Tampa Bay, Florida. Gillian, welcome.
Gillian Sealy: Good morning. Thank you for having me. I'm looking forward to this discussion.
Rhea Ramjohn: So, Gillian, before we talk about the “Thanks Birth Control Study” that your organization recently conducted, can you tell us who is most vulnerable to losing access to birth control and reproductive care right now?
Gillian Sealy: I think really and truly, we really need to understand what's at stake as it relates to reproductive health and sexual health and access to contraception. We do know that there was a vacancy on the Supreme Court, but I think it's much more than that. We also want to make sure as we look at policies that will be happening within the next few weeks and months around access to insurance, right? Because we know that having insurance allows people, in this particular case, young people and women, to be able to use their insurance care to access contraception. In addition, we want to make sure that at the federal and state level, there are policies that are supportive of reproductive health and sexual health, including contraceptive access and abortion.
Rhea Ramjohn: So we’re talking to you today because your organization, Power to Decide, did your annual Thanks Birth Control Survey. How have this year’s survey results compared to previous years? How has the pandemic affected birth control users?
Gillian Sealy: What we have seen and, you know, we did the Thanks Birth Control Survey about the impacts of COVID-19 and 80% of those polled, and these were birth control users 18 to 34, said that birth control has allowed them or their partner to worry about one less thing during the COVID pandemic. And 8% of those respondents said that they or their partner planned to get pregnant in the next 12 months. So the fact that 8% of respondents said that they or their partner planned to get pregnant in the next 12 months, suggests that there is a possibility that, you know, people are looking at LARCs and other forms of birth control to delay pregnancy over the long-term, especially as this pandemic continues to to rage on and we don't know when the pandemic will be over. So I think people are making plans for their lives around delaying pregnancy, delaying having a family and really thinking a lot more about their reproductive and sexual health lives during this pandemic.
Rhea Ramjohn: In the intro, I mentioned the vulnerability and instabilities that the pandemic has further exposed. So prior to the pandemic, how secure was birth control access in the U.S.?
Gillian Sealy: So pre-COVID, we were very concerned about access to contraception. For instance, women have always faced barriers when it comes to accessing contraception; whether those are financial barriers, lack of insurance, transportation, being unable to access child care, and these are just a few of the barriers that we know that women face. This is particularly hard for marginalized populations, women in poverty, women of color, women living in rural areas. So these were the things that we saw and we were acutely aware of pre-COVID. The pandemic has just exacerbated the lack of access for those people in particular. And Power to Decide has always been and continues to be concerned with how to make sure that people are still accessing the contraception in the middle of a pandemic, and what resources are the best for them so that they can get what they need.
Rhea Ramjohn: Mm-hmm. Obviously, security and vulnerability vary all over the world. So what's the frame that our worldwide listeners can think about when considering birth control access? For example, I would imagine that living in a country with universal health coverage would make access more secure, or am I wrong to assume that?
Gillian Sealy: The pandemic is global, right? The fact that it is considered a pandemic means that it's global. So regardless of where you are, with stay-at-home orders, closures of university health centers, concerns of being exposed to the virus, getting to a clinic to be able to access birth control has become even harder, especially for young people. When you couple that with widespread job loss due to COVID-19, which has left thousands of young people without health insurance or the necessary income to purchase contraception. It really has changed our approach to healthcare, and especially for women trying to avoid an unplanned pregnancy. Wanting to make sure that you have access to contraception is something that is top of mind for many of them and their partners.
Rhea Ramjohn: I just wanted to ask and follow up there— you mention young people specifically, is that because of job or economic insecurity, or the university closures like you just mentioned? Break that down for us.
Gillian Sealy: I think it's more than the economic factor. I think, you know, just having access again, being able to have face-to-face visits with your healthcare provider has just been very, very hard to come by, especially in places where you have safer-at-home or stay-at-home orders. So that has really made the barriers even harder for young people. And in fact, it has had young people really thinking about their reproductive health. For instance, whether they will delay having a child or having a pregnancy because of the access issues.
Rhea Ramjohn: So as the pandemic started to unfold, what were the concerns that Power to Decide, which is your organization, had?
Gillian Sealy: I think there were a few of them. We talked about the access issues, right, about folks being able to go in and get their birth control. But we also saw, for instance, since March, there were quite a few states who were using the pandemic to further restrict abortion access. We placed our efforts in informing people that abortion is legal in the United States and where they can access the full range of reproductive health services and methods in the pandemic with restrictions. So, for instance, there were eight states, Louisiana, Texas, Oklahoma, Tennessee, Alabama, Iowa, Ohio, and Arkansas, that use the COVID-19 pandemic as an excuse to ban abortion by deeming it a non-essential procedure. And as we know, abortion is indeed extremely time sensitive, especially in states with waiting periods and few providers. And while since March, most of these bans have expired or were defeated by legal challenges, we do know that abortion care continues to be under attack. And I can't reiterate that enough, abortion and abortion care is time sensitive, especially for women of low income, women who have to travel outside of their state to access abortion care. So these are some of the things from a policy perspective that we're very concerned about in addition to access in terms of transportation, child care, financial barriers, etc.
Rhea Ramjohn: Of course. So can you describe concretely for me how the pandemic has actually changed access to all those services you've just described?
Gillian Sealy: Absolutely. So as I mentioned, in terms of the pandemic: not having access to your provider, the closure of university health centers, people worrying about being exposed to the pandemic, widespread job loss. We did a poll and 80% of polled birth control users, 18 to 34, said that birth control allowed them and their partners to worry about one less thing during the pandemic. So if they don't have access to birth control, this is one more thing, in addition to all the things that I mentioned that are barriers that they have to worry about.
Rhea Ramjohn: Yes.
Gillian Sealy: You know, and as I mentioned, COVID-19 has really changed our approach to healthcare for women trying to avoid an unplanned pregnancy, including how to access contraception. And what we have seen is, for instance, that telehealth is really a viable option as it relates to providing access.
Rhea Ramjohn: You’ve mentioned Telehealth, which is kind of a catchall term that includes lots of different new and innovative ways of using electronic platforms, apps and video calls and the like to provide medical care as opposed to face to face meetings with a doctor or health care provider. So, Gillian, do you see telehealth as filling a gap?
Gillian Sealy: We do see telehealth as filling a gap, but I want to be careful here and point out that everyone doesn't have access to telehealth services, right? We do know that there are those who don't have stable Internet connections and so cannot access telehealth and we recognize that barrier. However, we do see telehealth as a viable option. It's gaining tremendous support not just among patients, but also among care providers. And it really is important to understand that the convenience and effectiveness of telehealth, again, are a viable option. But I would want to put a pin here to say that in addition to those not having stable Internet access to access telehealth, it's really important to understand that the effectiveness of telehealth can be, and is, experienced disproportionately among women with higher incomes. So, for instance, a recent survey that was released by Power to Decide shows that significantly more respondents with an annual household income of $50,000 or more understood what telehealth was; 69% of them reported being able to use telehealth and then 68% of them knew how to find a telehealth provider compared to women with household incomes under $50,000, right. And so for women with lower incomes, and that means those under fifty thousand, only 21% knew or understood what telehealth was. So I want to be very clear that while telehealth is a viable option, there's still many disparities that we're seeing around this issue.
Rhea Ramjohn: Yeah, that's very disconcerting. It's just another example of how this pandemic is exposing so many vulnerabilities that were already there before the pandemic. So can you explain that gap? Like what is the reason for that gap?
Gillian Sealy: I think there are many reasons for the gap. We have to be very clear that the pandemic just has exposed many of the barriers to contraception that we have seen pre-COVID, right. I think, you know, COVID has just shined a light on what a lot of these access issues were. In addition to the ones that I just mentioned, supportive policies that support birth control and contraceptive access, sexual and reproductive health are really a key to making sure that people have access. Another example would be [how] Medicaid coverage expansion allows access to health insurance coverage that can help more women access the most effective methods of contraception by again removing those cost barriers. And we know that Medicaid is a vital source of health coverage, including for contraception. However, 12 states still have not expanded Medicaid for low income adults as allowed for by the Affordable Care Act. So in addition to those barriers that I mentioned, they are barriers from the political standpoint that also make it very difficult for people to access contraception, and I think that we're mindful that some of this might happen post-COVID as well.
Rhea Ramjohn: Telehealth is just one of those things that’s so interesting, because it has the potential to really change, in an on-the-ground way, how people access care. And I don't want to stay on this topic for too long, because I do have a lot of questions about your study as well, but I have two really important follow up questions about this.
Do you think that doctors are making information about telehealth services available to patients and prospective patients? And also, what about pharmacist-prescribed birth control?
Gillian Sealy: Yes, so I think that both providers and patients see that telehealth is important, especially during this pandemic, to be able to access contraception. Definitely there is a need for additional information, and so Bedsider, which is our online birth control support network, where we provide resident information on all methods of birth control so that people can find a method that works best for them, especially during this time. We have been doing lots of work to provide information, not just to the patients, but also to care providers on telehealth and the best ways to be able to access it and the importance of it. So more information and education is clearly needed for both parties. And I will say that post-COVID, there is the possibility that patients and providers will want to see telehealth expanded to be able to serve their patients and allow for, again, greater access.
In terms of pharmacists prescribing, policies at the state level could make it harder or easier to access birth control over the counter. So, for example, currently there are 17 states, including the District of Columbia, that have enacted policies to allow pharmacists to prescribe and dispense self-administered hormonal methods. So that would include the pill, the patch, the ring, the shot. And so given this landscape, and ongoing federal policy challenges, interest in allowing pharmacists to prescribe hormonal contraception is likely to continue to gain traction in these states. In fact, new research from Oregon, California, Colorado, and Hawaii suggests that this model is helping to fill a gap.
Rhea Ramjohn: Gillian, we have a lot more to discuss about how this pandemic is affecting people’s access to reproductive care and birth control, but before we continue, let’s take a quick break.
Hormonal is brought to you by Clue: the period tracking app and menstrual health encyclopedia that takes your cycle seriously.
Clue has been around since 2012, and since then our community has grown to millions of people. And we want to be around for years to come.
But to do that, we need support from people like you. By subscribing to Clue Plus, you’re supporting the work here at Clue. You’re also keeping the app free for others who maybe don't have the same resources or access as you. And you’re helping fund important menstrual health research around the world.
To learn more about becoming a Clue Plus subscriber, go to Clue.plus.
Alright, back to the show.
Rhea Ramjohn: Welcome back to Hormonal. I’m your host, Rhea Ramjohn.
Gillian, as we all know, many of us first-hand, job instability and unemployment have increased over the course of the pandemic. In the US alone, there are millions without a job, and that’s, for a lot of people, their connection to their health insurance.
What does this mean for people who use birth control and their options?
Gillian Sealy: The pandemic has had devastating effects, not just from a health perspective, but also from an economic perspective as well, and has caused people to lose their jobs, which has had an impact not just on their insurance, but also being able to afford their contraception out-of-pocket. So it has had devastating effects for them as well. And thinking about how they will be able to afford their contraception again, you know, it is time sensitive. You want to make sure that people continue their method of birth control and it's even more important during this pandemic, as they are not able to go to their doctors to be able to get their contraception. So, to your point, not being able to have insurance adds another layer of the barriers that people are seeing, being able to afford healthcare, but in particular their contraception as well.
Rhea Ramjohn: You alluded to this in the “Thanks birth control” survey that a lot of people aren't looking to have a baby in the next 12 months, and I think this kind of flies in the face of this joke at the beginning of the lockdowns earlier this year, that there would be these so-called, quote unquote, lockdown babies. It can be funny for some and not for others. So what is your reaction to these kinds of assumptions?
Gillian Sealy: I think exactly as you just said, they're assumptions, right? And just like you, I heard all those jokes and suggestions that we will probably see a boom in COVID babies. But I think that when you dig deeper and you look at the surveys that we at Power to Decide have conducted and released, and other surveys, people are really thinking about their reproductive and sexual health and what that means for their future–for a number of reasons. The reason why there was that assumption that there would be a baby boom is because people were going to be at home, they were sheltering in place. But more importantly, along with this pandemic has come all the other things that we talked about: economic barriers with people losing their jobs and losing their health insurance, and that having a devastating effect on their families and really having them think a lot more carefully about what that means to their family formation. So I think that's one of the pieces and one of the places where we will find out, you know, nine months, one year from now whether that assumption holds true. But I think it's just much more multifaceted than saying that people are at home so in nine months we'll see a baby boom. I think people are just carefully thinking about how this pandemic is affecting their lives, not just in the moment, but also for their future as well.
Rhea Ramjohn: What do you recommend to people trying to minimize trips to the doctor's offices or in public in general, but still want access to birth control? What are our best bets?
Gillian Sealy: I think there are a couple of things that you can do. First and foremost, I encourage people to go to Bedsider.org, which is powered by Power to Decide where we continue to update and provide resonant information about telehealth, not just what telehealth is, but how to access telehealth. And I would also encourage folks to talk to their healthcare provider. Even if you are accustomed to having an in-person appointment with your doctor or your healthcare provider, this is a prime opportunity to have a conversation with them as to whether telehealth is a viable option for you. I would also encourage people to reach out if they have health insurance to their health insurer to see if telehealth is something that is covered under their health insurance as well.
Rhea Ramjohn: What do you think providers have learned over the course of this pandemic about how they can better offer care? What have been the innovations?
Gillian Sealy: Based on the pandemic and based on the fact that we just have not been able to do face-to-face appointments and being able to see our healthcare providers, we've seen a boom in telehealth, and I want to be clear that telehealth was an option before the pandemic. But I don't think that there was the added need as well as desire for folks to use telehealth as a viable option, and healthcare providers are also seeing a viable way to reach patients, especially those who are most marginalized. So those who are living in rural areas, in areas of poverty, and especially for people of color, I think this is a really viable option to reach those patients who need access to care. And when I say access to care, I anticipate that this will obviously be a lot greater than just contraception. So this is probably going to be a new way that we see healthcare taking off post-pandemic. And even when you look at policies that might be being enacted now to allow for telehealth due to the pandemic, I think after the pandemic there's going to be a groundswell, especially from patients and likely healthcare providers as well for this to continue. So I think for healthcare providers, they really see this as a solution to a complex problem in terms of healthcare.
Rhea Ramjohn: You touched on this, but in general, are there changes that have come from the pandemic that you think are here to stay?
Gillian Sealy: The option of telehealth is something, in terms of whether we will see policies about how telehealth is enacted, that is something that we will see more of. It will be left to see, in terms of insurance companies, what their thinking is around telehealth and being able to offer that as a standard option for patients. Being able to use something like telehealth as a resource, for instance, to get birth control delivered to your door in a pandemic, is something that we will probably continue to see more of. As we talk about pharmacy prescribing, we will likely see, in addition to those 17 states, maybe other states who are also going to be thinking about that, because this goes much further than allowing for access during the pandemic, but allowing for access in general, especially for those for whom access has traditionally been and continues to be a major barrier.
Rhea Ramjohn: Mm-hmm. Gillian, 2020 has been hard to put into words. Let's just say it's been a tough year and it's likely that we won't see a resolution to the pandemic any time soon. So what is your big message to listeners who are worried about their own access, or access for others?
Gillian Sealy: There's no end in sight at this point, in terms of the pandemic, on what that looks like for millions of people across the world for access. Access was an issue for various populations before the pandemic, but this really shone a light, not just for individuals and the healthcare profession, but also policymakers and advocates, that we need to focus on access and what access looks like, and how we can make sure that all people have the access to the healthcare that they need, including for contraception and abortion care. COVID-19 has changed our approach at this point in time for how women, for instance, avoid an unplanned pregnancy, and this includes access to contraception. I will say that the pandemic has allowed us to look at telehealth as a viable option, [as well as] delivered-to-your-door contraception. And because we don't know when the pandemic will end, I suspect that we will continue to see these options and these topics being more focused on as we ride through this pandemic, but more importantly, after this pandemic is over, I suspect that we will continue to see calls for things like telehealth being more mainstream so that people have the access that they need.
Rhea Ramjohn: Gillian, we’ve talked a lot about the Thanks Birth Control Survey, and we have a link to that survey in the show notes. What jumped out to me is that there seems to be reasons for us to be optimistic. Could you expand on that for us?
Gillian Sealy: Absolutely, and in this survey, we specifically asked about the impacts of covid, and some of the top line things that we were able to glean from the survey is that 80% of polled birth control users, aged 18 to 34, said that birth control has allowed them and their partner to worry about one less thing during the covid pandemic, right, and as we talked about, there are many things to worry about during the covid pandemic. But this allows them to worry about one less thing. 82% of respondents, 18 to 34, said that they had access to accurate and reliable information about birth control, and we definitely know that this is really important because it allows people to get all the information that is resonant and accurate and then make an informed decision for themselves around their method of birth control.
Gillian Sealy: 94% percent of respondents, again, age 18 to 34 who use birth control, are actually thankful that birth control has allowed them or their partner to decide if or when to have a child. But again, we talked about during this pandemic how people are thinking about delaying having children or are thinking more about their reproductive and sexual lives. And so 94% of respondents were thankful for birth control that allows them to do this is a really good thing. And then 84% of respondents, 18 to 34, who use birth control are also thankful that birth control has allowed them or their partner the ability to work towards their professional and educational goals. So there is and are glimmers of hope during this pandemic. I would be remiss if I didn't also reveal one or two other things from the survey. So, for instance, 18% of respondents aged 18 to 34, reported that they were unable to see their provider for sexual and reproductive healthcare in person during the covid-19 pandemic. And this really highlights the importance of finding solutions for folks who are wanting to access contraception during this time and I go back to telehealth solutions, delivery to your door of hormonal contraception and others that make access much more viable during this time.
Rhea Ramjohn: Gillian Sealy is the interim CEO of Power to Decide, and she joined us from Tampa Bay, Florida. Gillian, thanks so much for making time for us today on Hormonal.
Gillian Sealy Thank you so much for having me.
Credits
Rhea Ramjohn: Hormonal is hosted by me, Rhea Ramjohn! Our Executive Producer is Kassandra Sundt.
Editorial help from:
Amanda Shea
Steph Liao
Nicole Leeds
Special thanks to:
Marta Pucci
Trudie Carter
Maddie Sheesley
Ryan Duncan
Aubrey Bryan
Claudia Taylor
Léna Calvarin
Lynae Brayboy
Yomi Eluwande
And Jane Parr-Burman
Mixing and recording help from Bose Park Productions and Rekorder Studios in Berlin.
Thanks for listening to Hormonal. Please rate and subscribe, and tell a friend! Until next time, I’m Rhea Ramjohn.