


A podcast about how hormones shape our world.
Latest episode:
Who you gonna call? Mythbusters!
About Hormonal
Hormones affect everyone and everything: from skin to stress to sports.
But for most of us, they're still a mystery.
Even the way we talk about hormones makes no sense. ("She's hormonal.")
So let's clear some things up. Each week, Rhea Ramjohn is asking scientists, doctors, and experts to break it all down for us.
Subscribe on your favorite platform:
Episodes
- Season 1
- Season 2

Episode 0
August 25, 2020
A Sneak Peek at Season 2
As we work hard on Season 2 of the Hormonal podcast, we’re dropping into your feed with a special request, and a small behind the...
5 min

Episode 1
October 11, 2020
Hot or not? Birth control & sex drive
How birth control affects your sexual desire, self image, and weight fluctuations.
25 min
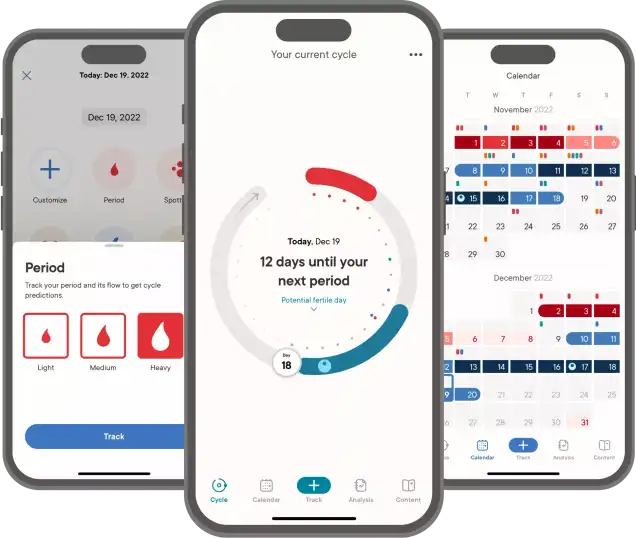
Support Hormonal & the period tracker that’s different from the rest.
Subscribe to Clue Plus
Episode 2
October 19, 2020
The ABC: Abortion & Birth Control
What’s it like to get an abortion and the surprising ways the pandemic is changing abortion access.
34 min

Episode 3
October 26, 2020
The many sides of side effects
Hormonal birth control: positive, negative, and neutral effects
33 min
Support Hormonal & the period tracker that’s different from the rest.
Subscribe to Clue Plus
Reproductive choice and reproductive justice
with Dr. Loretta Ross
Episode 4
November 2, 2020
Reproductive choice and reproductive justice
Accessing birth control against the odds
35 min

Episode 5
November 9, 2020
Happy birthday, birth control
Controversy and celebration on the 60th anniversary of the pill
42 min


Episode 7
November 23, 2020
Risky business: birth control during COVID-19
COVID-19 is changing how we access birth control
30 min
Support Hormonal & the period tracker that’s different from the rest.
Subscribe to Clue Plus
Who you gonna call? Mythbusters!
with Lynae Brayboy, Amanda Shea & Hajnalka Hejja
Episode 8
November 30, 2020
Who you gonna call? Mythbusters!
Clue’s Science Team busts your birth control myths
37 min
Credits
Season 2
Executive Producer: Kassandra Sundt
Host: Rhea Ramjohn
Editorial Help from: Amanda Shea, Steph Liao, Nicole Leeds
Clue Design: Marta Pucci & B.J. Scheckenbach
Web Team: Yomi Eluwande, Jane Parr-Burman, Maddie Sheesley
Special Thanks: Trudie Carter, Ryan Duncan, Aubrey Bryan,
Claudia Taylor, Léna Calvarin, Lynae Brayboy
Mixing and recording help from: Bose Park Productions & Rekorder Studios in Berlin.
About Clue
Clue is a period tracking app that uses data and science to help women and people wih cycles to understand their bodies. It's also a menstrual and reproductive health encyclopedia.
Learn more about the Clue app and check out what Clue is doing to advance menstrual health research.


Rhea Ramjohn,
host of the Hormonal Podcast


Rhea Ramjohn,
host of the Hormonal Podcast
Your Host
The more knowledge we have about our hormones, our medical & menstrual care, and our reproductive rights, the more we empower ourselves and one another.
Hormonal has offered me the true privilege of speaking with people who have the expertise on the scientific knowledge about our hormones and cycles, as well as those sharing their lived experiences, caring for people with menstruation and how, all combined, shapes our lives everyday.
Gathering facts as well as personal stories are so vital to our understanding of our health, our his/herstories, and our cultures. I deem it a privilege because we haven't had many platforms nor opportunities for menstrual health information being broadly accessible.
Episode 6
Bringing sexy back
About
Pregnancy causes big changes in your body, both hormonal and physical. Midwives Imogen Raye Minton and Yasmeen Bruckner join us this episode to explain what people who’ve just had a pregnancy need to consider about their birth control options afterwards.
Transcript
This transcript and interview were edited for clarity.
On Hormonal we explore the science behind hormones. But we also talk about society and the world around us. On Hormonal, we know that there are lots of women who have periods and lots who don’t. We also know that there are people who aren’t women who have periods too. We also know we have listeners who have never had periods. We hope you feel welcome, even when a term that a guest uses maybe doesn’t apply to you.
At Clue, we believe that our identities are not determined by our bodies. Thanks for listening to Hormonal.
Rhea Ramjohn: Hi, I'm Rhea Ramjohn. And you're listening to Hormonal, brought to you by Clue, the menstrual health app.
This season on Hormonal, it's all about birth control. And today, we're going to be talking about birth control during a phase in life that might seem contradictory to some: right after a pregnancy. A pregnancy, as we know, brings along big changes to someone’s body. Hormones like estrogen and progesterone rise... and there’s an increase in breast milk creating hormone, on top of the physical changes already happening to your body.
So what do people who’ve just had a pregnancy, whether it ended with a baby or not, need to know about their birth control options afterwards?
To discuss this, we have a very exciting conversation with two midwives from nearly opposite sides of the planet. Joining me here in Berlin is Imogen Raye Minton, a home birth midwife and co-founder of the Queer Feminist Midwifery Collective. Imogen, welcome.
Imogen Raye Minton: Hi, it's so nice to be here.
Rhea Ramjohn: And joining us on the line from Seattle, Washington is Yasmeen Bruckner. Yasmeen is a certified nurse, midwife and women's nurse, and health practitioner at the University of Washington Northwest Campus Midwives Clinic. Yasmeen, Thanks for joining us.
Yasmeen Bruckner: Thank you so much for having me.
Rhea Ramjohn: Well, I'm really excited for this conversation today, and I hope we can all be in conversation about this topic. I might direct a question to one of you specifically, but also feel free to chat between one another. But, Imogen, I'm going to start with you.
I mentioned a bit in the intro about the hormonal changes that someone might experience during a pregnancy, but let’s talk a bit more about these changes. What are the other physical changes that someone might experience?
Imogen Raye Minton: Sure. Some of the things have to do with healing and returning to kind of near the original state of the organs, you know, you have the uterus which grows to many times its original size and goes from being the size of a fist to the size of a watermelon. All of those additional muscle cells and the supporting connective tissues have elongated exponentially in an incredibly short amount of time and then return to close to their original positions. And also in a relatively short amount of time, the other organs that have made space for this growth are slowly descending back into their comfortable places. And the pelvic floor is, as are the muscles of the stomach, coming back together after they've also become more elastic and spread apart to allow both the growth of the pregnancy and for a baby to to exit the body.
Rhea Ramjohn: Do hormonal changes or physical changes of the body differ between someone who’s had a full term pregnancy that ended with a birth compared to someone who’s had a termination or a miscarriage?
Yasmeen Bruckner: That's a good question. So it is a little bit different. The hormone changes that happen after, say, a full term pregnancy vs. a first trimester miscarriage -- in fact, the body goes back to cycling that ovulatory cycle relatively quickly after a first trimester miscarriage. Versus after full term pregnancy, a lot of people, especially people who are choosing to breastfeed their child, [find] that they do not go back to an ovulatory cycle for potentially many months and potentially longer than that, and that part is because of the the role of prolactin in suppressing ovulation.
Rhea Ramjohn: Right, but breastfeeding is not a guarantee, because, of course your ovulation will come back before your menstruation.
And actually, a question for both of you: so, let's say a pregnancy is not brought to full term. Does that actually also have an affect on how the hormonal cycle changes? And how the body changes?
Yasmeen Bruckner: So that return to the ovulatory cycle is the same in both cases. It doesn't matter how the pregnancy ends.
Rhea Ramjohn: Imogen. Yasmeen kind of alluded to this, but perhaps you can spell this out for us. How quickly after a pregnancy can someone become pregnant again?
Imogen Raye Minton: So I think, well, first I want to say full disclosure, that I slept maybe two hours last night because of a birth. So if I don't make sense, please let me know. But I'm going to take a stab at it.
Yasmeen Bruckner: I'm in the same position, so I totally understand. [Laughter].
Rhea Ramjohn: Life does not care about the midwife schedule. Well, thank you both for being here and for all your energy. Thank you.
Imogen Raye Minton: Well, it's great to get to talk to a midwife who's working in the U.S. system. So, I think that this is where there's a lot of work that our bodies do for us to try to protect us from a quick succession of pregnancies. It's really great if the body can go through a complete involution cycle, which is just like the uterus returning to close to its original size and a lot of other readjustments after birth. So that's one of the reasons, evolutionarily, that prolactin suppresses ovulation. And also if you're chest feeding or nursing. And also this drop in progesterone and estrogen for a lot of people causes also a pretty significant drop in their libido. So nature is doing a lot of stuff to try to keep us from getting pregnant too quickly after a birth. And yet there is always the possibility that within weeks of giving birth, it is possible to ovulate, especially if you're not lactating. And I think that there it's important to note that the first ovulation happens before the first menstruation. So you actually have no idea, unless you're very sensitive, and you can feel your ovulation, whether or not you're ovulating. There's no cycle to track at that point.
Rhea Ramjohn: So definitely you all are having different experiences operating in different medical systems in different parts of the world. So I'm really curious to find out what birth control method is most common after a full term pregnancy. Would what do each of you actually like to recommend to your clients?
Imogen Raye Minton: I can go first here. I feel like my position is a little bit different than Yasmeen's, because I know that in the U.S., midwives are allowed to do more sort of generalized fertility based health care. In Germany, that's an area that is very off limits for midwives. So we can't, for example, insert IUDs and we can't do pap smears. We can't do IUIs, which is intrauterine inseminations. But that aside, I think that in general, I still do do some contraceptive counseling at the end of every postpartum period with my clients. And I would say that because I work with a very broad group of people, my advice is very client centered and ranges from, you know, whether they're looking to prevent conception, in which case my two main recommendations are barrier methods or an IUD, a copper IUD.
If they're looking to postpone future pregnancies for longer than a year or two at a time, and they don't have any of the risk factors that would make a copper IUD a bad idea, and for many folks who are having sex in a context where conception is not an issue, they still might have interest in different barrier methods, or different methods of having safer sex with their partner or other partners after birth, especially during the period where the postpartum bleeding is happening.
Rhea Ramjohn: Right. And for our listeners, could you give us specific examples of what the barrier methods are?
Imogen Raye Minton: Sure. So, for example, if you're having a really heavy postpartum bleed and you want to have oral sex, for example, some people find it comfortable to use a dental dam. Also, using gloves for digital sex can be really nice and is also a way to, I think, be gentle with with the tissues that might be a bit more sensitive. "A bit more sensitive" is maybe an understatement after you've given birth. I think that, for many people, having protection for fingernails, for example, can feel really nice when their body is feeling pretty sensitive.
Rhea Ramjohn: For sure. Very good point. And for people who may not know, a Dental Dam is a kind of barrier used most often for oral sex. We’ll put a link to that in the show notes.
And what about you, Yasmeen. What kinds of birth control methods do you speak about with your clients after pregnancy?
Yasmeen Bruckner: Yeah... I feel really fortunate that I am able to offer people a wide variety of options. In the United States, midwives are trained and our licensure allows us to provide all forms of hormonal and non hormonal contraception. And the things that we don't do are really just the permanent options for contraception. So that means a vasectomy or a tubal ligation. Those are really the only two things that I can't offer to my clients, which is pretty awesome.
Imogen Raye Minton: God. That's so cool. Yasmeen, I just think that's such a smart system, you know, where you can really be a holistic care provider.
Yasmeen Bruckner: It really does feel as though it's providing continuity of care so that this person, this family that has entrusted you during their pregnancy and during their birth are then able to get what they need for the next phase. In the same place and from the same people. And I think that's really a service to the community. But to go to your question, which is what do I talk to people about - I talk to people about both non-hormonal options and progesterone-only options for people who are choosing to nurse their babies. I try to really tailor how I counsel people to what it is that they're in need of and what it is that they're looking to get out of their birth control. So I will say that for a lot of people, their goal is to prevent another pregnancy, maybe in the short term or maybe in the long term. And so if the goal is to consider having another baby relatively soon, then something like barrier methods, as Imogen spoke of it, can be really a nice option because they're not a long term commitment with something like a condom. Right? And you can choose whenever you're ready to stop using that, if you're wanting to conceive. I also offer people some progesterone-only option that's in a pill form. Again, that's a really nice choice because you can stop it at any time on your own. There are also IUD that I offer people in the postpartum period. I offer both the hormone-based IUD, because they have progesterone in them, and I also offer the copper IUD, or the non hormonal IUD, as well.
Rhea Ramjohn: So this is a really important conversation and I want to continue on this topic. But before we continue, we're going to take a quick break.
Hormonal is brought to you by Clue. The period tracking app, and menstrual health encyclopedia, and now, a pregnancy tracker!
You heard that correctly! Clue is launching our most requested feature ever: Clue Pregnancy mode! Now, you can track your pregnancy symptoms, get scientifically-backed information on how your body is changing each week, and follow your baby’s growth from conception to birth to post pregnancy.
If you’ve been using Clue as a period tracker, all you need to do is subscribe to Clue Plus, go to settings, and switch to Clue Pregnancy mode. Clue Pregnancy mode is available on Android today, and coming to Apple devices by the end of 2020.
Alright, back to the show.
Rhea Ramjohn: You're listening to hormonal. I'm Rhea Ramjohn.
You know, I’m curious about how the post-partum care differs between Germany and the US. Could you tell me a bit more about this? Imogen?
Imogen Raye Minton: Here in Germany, we have a really comparatively very, very supportive postpartum system where your midwife can visit you every day, every other day for multiple months, and you're protected by law to have at least two months postpartum off and, following up to a year and a couple months even beyond, paid for at least part of your original salary by the health insurance company and the government. And so there's a lot of support for people to be able to really rest during that period as much as you can rest when you have a baby and to allow this sort of process of your body returning to its nonpregnant state to happen in a healthy way. And I think that Yasmeen might experience that differently in the U.S., where there's really no strong federal postpartum protections. Is that the case?
Yasmeen Bruckner: That's really true. And it's actually... it's very challenging. We spend a lot of focus on pregnancy, but there is much less support here in the United States for postpartum care. There are no programs that allow people to be home more than maybe a couple of weeks. I live in a state where we're ahead of the curve or we're ahead of the rest of the country, I think, in having paid parental leave. Washington state now has a program for paid parental leave, which is about 12 weeks for most people. And either the birthing parent and the non birthing parent can take that time. But that is an anomaly here in this country. I work in a hospital setting. There are midwives who work at home and in birth centers. And so they will do home visits. But for my clients, I see them for a two week visit and a six week visit. More visits in between if needed. And then maybe a contraception visit after that. But then really in terms of support, that's it. Which is which is fine for some people, and it can also be really hard for others.
Rhea Ramjohn: So this is exactly why we find this conversation about midwifery and birth control interesting and the intersection of that, because as Imogen pointed out in Germany, you have so much postpartum care. It was the very first time that I had learned that midwives are a part of your postpartum care. I thought it all ended with the delivery of the baby. So thinking about that, and you've both mentioned this lifestyle post-delivery, this new addition to one’s lifestyle - what kind of advice would you give parents that they should know about their lifestyle, how that may change, and especially including birth control? At this time?
Imogen Raye Minton: I'm going to jump right in because I really like this topic. [Laughter] You know, my impression is we don't have a lot of very clear models of what early parenthood looks like. And I think that the models that we do have are incredibly hetero-normative and incredibly cis-normative.
I think that as our family has gotten more nuclear, we have less support structures. People are left more and more to their own devices in a situation where especially if -- and honestly, not to plug my job, but midwives are absolutely vital postpartum -- especially in contexts where they don't have midwifery support or, let's just say, any kind of knowledgeable regular guidance that they don't have to pay for out of pocket, but that's covered by insurance, I think that many people end up feeling incredibly overwhelmed. There's very high anxiety levels. There's higher chances of postpartum depression, both for the parent who gave birth and also for the parent that didn't or the parents that didn't. I think that also, if your family's structure doesn't fit into that kind of normative model, you might really struggle to figure out what you're supposed to be doing. You know, media isn't much help and online forums are a total wash. So I think that people feel really isolated. Sometimes! People can feel really isolated. They can feel like they don't have the information that they need to feel safe. And I think that, in combination with the fact that you're experiencing usually pretty significant sleep deprivation with a new baby, and if you're feeding the baby from your body, you're experiencing the effects of prolactin and also oxytocin when you are nursing or chest feeding or body feeding. These hormones are hormones that make you feel bonded and cuddly, they're not the kind of hormones that make you feel really enthusiastic about having -- everybody's different -- but having wild sex in the shower or something while the baby's sleeping, you know, I think a lot of people feel really touched out. I think a lot of people feel overwhelmed. And I think that those things are really normal.
But, in our culture, there's not a lot of conversation around it. And so I think that can feel really like you're faulty, like you're not functioning properly if you're not really enthusiastic about having sex postpartum. If your body doesn't feel familiar to you. If it feels like it's kind of at the beck and call of this other new little being, or if you feel like you're constantly doing chores and and other sort of reproductive work to support your partner who's busy feeding the baby, all of these things can create a situation where, for many people, contraception is not super high in their minds, but rather this feeling of pressure and disconnect surrounding sex and sexuality in general. I want to specify that while that's true for some, it's not true for others. Some people have super adventurous, very exploratory, fabulous sex lives shockingly quickly after giving birth. And that's fantastic, too. I just think that we don't talk about either of those things very much. And that's missing for me. That to me feels more important, having those conversations with my clients, separate from a conversation like... contraception is not more important to me than having that conversation about sexuality in general.
Rhea Ramjohn: So, Yasmeen, what do you recommend to people who are post-termination or post-miscarriage in terms of birth control? And how do you approach these conversations differently than, let's say, a pregnancy that leads to birth?
Yasmeen Bruckner: So I think the way that I start is a conversation about that person's fertility goals. We cannot assume that because somebody had a termination of pregnancy that that wasn't a desired pregnancy or that they don't desire pregnancy. And just because somebody has had a spontaneous miscarriage, it doesn't mean that that was a desired pregnancy either. So the first thing that I try really hard not to do is to make an assumption about where that person is and to have a conversation with them. What is it that you are hoping for? What is it that I can offer to you? Some people who've had a miscarriage, they don't feel ready to start trying right away. And so they do want something for contraception because while they may be ready to have sex again, they are not ready to start walking through the journey of pregnancy again. Other people who've had a miscarriage want to be able to try for pregnancy right away. And so in those situations, I don't counsel people that they have to wait or that they have to use contraception for three months or six months, which was kind of an old school thing that was happening in our country for reasons that are unclear to me. So I think that that's the approach I take: what is the goal? Somebody who doesn't want children right now, doesn't want a pregnancy right now, they have a whole range of choices. Every option is on the table for them, for contraception. And they can start that at the time of a miscarriage, at the time of a termination, so long as everything was normal and uncomplicated.
Imogen Raye Minton: I really agree with that. I just want to jump in there and say that I love the thing with this question, what kind of contraception do you recommend? You keep coming back to the answer: it's highly individual. And I think that is such an important tenet of many different kinds of health support. And I would say especially of midwifery care - IUDs are a good option for people who are in the position that Yasmeen was talking about, of really looking for a highly effective, longer term method with limited side effects. And I also am grateful that there is a method on the market that I can recommend where people can be so spontaneous, you know, if you decide that you don't want to be pregnant for four years and then, from Friday to Monday, you decide you do, you can have the IUD removed. And if it's a copper IUD, there are no lingering hormonal shifts. And for many people, it's possible to get pregnant immediately after removal. So it's a very flexible method.
Rhea Ramjohn: And I feel like we haven't explicitly said this, but from what I understand, people can get an IUD placed right away after a birth or maybe start the pill or another method right away after pregnancy. And also, when do these non-barrier methods come up?
Yasmeen Bruckner: I typically try to wait until the uterus is healed before initiating contraception, especially something like an IUD where there is the higher rate of the IUD coming out on its own if it's placed in the immediate postpartum period. But unfortunately, in our country, there are people who don't have great access to health care, or there are other barriers to getting health care in the postpartum period, and there are times where I do think that it is reasonable to give somebody an IUD immediately after the placenta comes out or to give somebody a birth control pill or birth control shot or an implant in their arm before they leave the hospital because they want contraception, they don't want to get pregnant right away, and they may not be able to come back for health care, or they may be in a situation where they could potentially get pregnant before they come back to get their contraception. So based on the setting that I work in, it's not something that I do often, but it is something that I do like to have the option that it can be really valuable for people.
Rhea Ramjohn: So we’re going to be doing a whole episode on Mythbusting on a future episode, but since you’re both so knowledgeable and have already busted some myths of my own today, and maybe just because I have it on the brain, I’m wondering if you both have myths you come across often that you’d like to bust and tell us the real deal? Do you have any myths?
Imogen Raye Minton: I think the myth that I'd most love to bust is that giving birth to a baby through the vagina somehow stretches you out and destroys your ability to feel pleasure. I think that that is such a pervasive myth for folks that they, in this stage of healing after birth, feel like one of the things that they're grieving is the loss of their previous sexuality. Like the way that things felt, the way that that clitoral stimulation feels, the way that penetration feels. And I just want to say that I have had equal experiences of folks who say their sexuality has blossomed postpartum and they have stronger orgasms that they can feel their whole clitoris, that they have much more focused pelvic floor control after they've done their wonderful pelvic floor classes and therefore can enjoy penetration in a different way. And I think another thing I want to point out is that some people have luck if they weren't previously able to ejaculate or squirt, doing that. And so there's just this incredible adventurous, you know, landscape ahead to explore either by yourself or with a partner or with multiple partners. And I think finding a method of having safer sex or using contraception that feels really empowering can be a very important part of making that feel fulfilling and satisfying.
Rhea Ramjohn: Oh, that's some of the best myth busting I've heard recently. Thanks for that! And Yasmeen, last but not least, what is a myth that you bust commonly?
Yasmeen Bruckner: Yeah. Yeah, such a good question. I have. I really try hard to bust the myth about “six weeks”, and I don't know if this is a myth in Germany, too. But there is this thing, this idea, that everything should be back to normal by six weeks. And I really try to encourage people to think about how long it took them to grow a baby in their body and the incredible feat it is to birth a baby no matter how you birth your baby. And then now for milk production to totally ramp up and be able to feed that baby, you know, maybe as the primary source of food for that baby, to just honor all of those transitions and to be kind to your body. I think the images that we get in the media of what women's bodies, what birthing people's bodies, should look like after they have a baby, six weeks later, is completely unrealistic. And it doesn't honor what the body's done. Some people are ready to have sex again, are ready to exercise again. But a lot of people are exhausted. Sex does not sound appealing, and that is totally 100 percent ok and normal.
Imogen Raye Minton: That's beautifully put.
Rhea Ramjohn: Wow. That’s perfectly said. I think that’s a great place for us to stop. I would like to say, Yasmeen Bruckner, who joined us from Seattle, Washington, Yasmeen is a certified nurse, midwife and women's nurse, health practitioner at the University of Washington Northwest Campus Midwives Clinic. Yasmeen, thank you so much for joining us.
Yasmeen Bruckner: Thank you so much for having me. It was a pleasure to be with you all this morning.
Rhea Ramjohn: And Imogen Raye Minton is a home birth midwife and co-founder of the Queer Feminist Midwifery Collective here in Berlin. Imogen joined us here in the studio, and thank you so much for joining us on the podcast as well.
Imogen Raye Minton: It's my pleasure. Thanks for hosting this.
Credits
Rhea Ramjohn: Hormonal is hosted by me, Rhea Ramjohn! Our Executive Producer is Kassandra Sundt.
Editorial help from:
Amanda Shea
Steph Liao
Nicole Leeds
Special thanks to:
Marta Pucci
Trudie Carter
Maddie Sheesley
Ryan Duncan
Aubrey Bryan
Claudia Taylor
Léna Calvarin
Lynae Brayboy
Yomi Eluwande
And Jane Parr-Burman
Mixing and recording help from Bose Park Productions and Rekorder Studios in Berlin.
Thanks for listening to Hormonal. Please rate and subscribe, and tell a friend! Until next time, I’m Rhea Ramjohn.
Related links:
https://helloclue.com/articles/life-stages/postpartum-sex-fertility-and-contraception
https://helloclue.com/articles/about-clue/how-to-use-the-clue-app-to-help-you-become-pregnant
https://helloclue.com/articles/pregnancy-birth-and-postpartum

Episode 6
November 16, 2020
Bringing sexy back
Birth control after a pregnancy
About
Pregnancy causes big changes in your body, both hormonal and physical. Midwives Imogen Raye Minton and Yasmeen Bruckner join us this episode to explain what people who’ve just had a pregnancy need to consider about their birth control options afterwards.
"There is this like this thing, this idea, that everything should be back to normal by six weeks. And I really try to encourage people to think about how long it took them to grow a baby in their body and the incredible feat it is to birth a baby."
On Hormonal we explore the science behind hormones. But we also talk about society and the world around us. On Hormonal, we know that there are lots of women who have periods and lots who don’t. We also know that there are people who aren’t women who have periods too. We also know we have listeners who have never had periods. We hope you feel welcome, even when a term that a guest uses maybe doesn’t apply to you.
At Clue, we believe that our identities are not determined by our bodies. Thanks for listening to Hormonal.
Rhea Ramjohn: Hi, I'm Rhea Ramjohn. And you're listening to Hormonal, brought to you by Clue, the menstrual health app.
This season on Hormonal, it's all about birth control. And today, we're going to be talking about birth control during a phase in life that might seem contradictory to some: right after a pregnancy. A pregnancy, as we know, brings along big changes to someone’s body. Hormones like estrogen and progesterone rise... and there’s an increase in breast milk creating hormone, on top of the physical changes already happening to your body.
So what do people who’ve just had a pregnancy, whether it ended with a baby or not, need to know about their birth control options afterwards?
To discuss this, we have a very exciting conversation with two midwives from nearly opposite sides of the planet. Joining me here in Berlin is Imogen Raye Minton, a home birth midwife and co-founder of the Queer Feminist Midwifery Collective. Imogen, welcome.
Imogen Raye Minton: Hi, it's so nice to be here.
Rhea Ramjohn: And joining us on the line from Seattle, Washington is Yasmeen Bruckner. Yasmeen is a certified nurse, midwife and women's nurse, and health practitioner at the University of Washington Northwest Campus Midwives Clinic. Yasmeen, Thanks for joining us.
Yasmeen Bruckner: Thank you so much for having me.
Rhea Ramjohn: Well, I'm really excited for this conversation today, and I hope we can all be in conversation about this topic. I might direct a question to one of you specifically, but also feel free to chat between one another. But, Imogen, I'm going to start with you.
I mentioned a bit in the intro about the hormonal changes that someone might experience during a pregnancy, but let’s talk a bit more about these changes. What are the other physical changes that someone might experience?
Imogen Raye Minton: Sure. Some of the things have to do with healing and returning to kind of near the original state of the organs, you know, you have the uterus which grows to many times its original size and goes from being the size of a fist to the size of a watermelon. All of those additional muscle cells and the supporting connective tissues have elongated exponentially in an incredibly short amount of time and then return to close to their original positions. And also in a relatively short amount of time, the other organs that have made space for this growth are slowly descending back into their comfortable places. And the pelvic floor is, as are the muscles of the stomach, coming back together after they've also become more elastic and spread apart to allow both the growth of the pregnancy and for a baby to to exit the body.
Rhea Ramjohn: Do hormonal changes or physical changes of the body differ between someone who’s had a full term pregnancy that ended with a birth compared to someone who’s had a termination or a miscarriage?
Yasmeen Bruckner: That's a good question. So it is a little bit different. The hormone changes that happen after, say, a full term pregnancy vs. a first trimester miscarriage -- in fact, the body goes back to cycling that ovulatory cycle relatively quickly after a first trimester miscarriage. Versus after full term pregnancy, a lot of people, especially people who are choosing to breastfeed their child, [find] that they do not go back to an ovulatory cycle for potentially many months and potentially longer than that, and that part is because of the the role of prolactin in suppressing ovulation.
Rhea Ramjohn: Right, but breastfeeding is not a guarantee, because, of course your ovulation will come back before your menstruation.
And actually, a question for both of you: so, let's say a pregnancy is not brought to full term. Does that actually also have an affect on how the hormonal cycle changes? And how the body changes?
Yasmeen Bruckner: So that return to the ovulatory cycle is the same in both cases. It doesn't matter how the pregnancy ends.
Rhea Ramjohn: Imogen. Yasmeen kind of alluded to this, but perhaps you can spell this out for us. How quickly after a pregnancy can someone become pregnant again?
Imogen Raye Minton: So I think, well, first I want to say full disclosure, that I slept maybe two hours last night because of a birth. So if I don't make sense, please let me know. But I'm going to take a stab at it.
Yasmeen Bruckner: I'm in the same position, so I totally understand. [Laughter].
Rhea Ramjohn: Life does not care about the midwife schedule. Well, thank you both for being here and for all your energy. Thank you.
Imogen Raye Minton: Well, it's great to get to talk to a midwife who's working in the U.S. system. So, I think that this is where there's a lot of work that our bodies do for us to try to protect us from a quick succession of pregnancies. It's really great if the body can go through a complete involution cycle, which is just like the uterus returning to close to its original size and a lot of other readjustments after birth. So that's one of the reasons, evolutionarily, that prolactin suppresses ovulation. And also if you're chest feeding or nursing. And also this drop in progesterone and estrogen for a lot of people causes also a pretty significant drop in their libido. So nature is doing a lot of stuff to try to keep us from getting pregnant too quickly after a birth. And yet there is always the possibility that within weeks of giving birth, it is possible to ovulate, especially if you're not lactating. And I think that there it's important to note that the first ovulation happens before the first menstruation. So you actually have no idea, unless you're very sensitive, and you can feel your ovulation, whether or not you're ovulating. There's no cycle to track at that point.
Rhea Ramjohn: So definitely you all are having different experiences operating in different medical systems in different parts of the world. So I'm really curious to find out what birth control method is most common after a full term pregnancy. Would what do each of you actually like to recommend to your clients?
Imogen Raye Minton: I can go first here. I feel like my position is a little bit different than Yasmeen's, because I know that in the U.S., midwives are allowed to do more sort of generalized fertility based health care. In Germany, that's an area that is very off limits for midwives. So we can't, for example, insert IUDs and we can't do pap smears. We can't do IUIs, which is intrauterine inseminations. But that aside, I think that in general, I still do do some contraceptive counseling at the end of every postpartum period with my clients. And I would say that because I work with a very broad group of people, my advice is very client centered and ranges from, you know, whether they're looking to prevent conception, in which case my two main recommendations are barrier methods or an IUD, a copper IUD.
If they're looking to postpone future pregnancies for longer than a year or two at a time, and they don't have any of the risk factors that would make a copper IUD a bad idea, and for many folks who are having sex in a context where conception is not an issue, they still might have interest in different barrier methods, or different methods of having safer sex with their partner or other partners after birth, especially during the period where the postpartum bleeding is happening.
Rhea Ramjohn: Right. And for our listeners, could you give us specific examples of what the barrier methods are?
Imogen Raye Minton: Sure. So, for example, if you're having a really heavy postpartum bleed and you want to have oral sex, for example, some people find it comfortable to use a dental dam. Also, using gloves for digital sex can be really nice and is also a way to, I think, be gentle with with the tissues that might be a bit more sensitive. "A bit more sensitive" is maybe an understatement after you've given birth. I think that, for many people, having protection for fingernails, for example, can feel really nice when their body is feeling pretty sensitive.
Rhea Ramjohn: For sure. Very good point. And for people who may not know, a Dental Dam is a kind of barrier used most often for oral sex. We’ll put a link to that in the show notes.
And what about you, Yasmeen. What kinds of birth control methods do you speak about with your clients after pregnancy?
Yasmeen Bruckner: Yeah... I feel really fortunate that I am able to offer people a wide variety of options. In the United States, midwives are trained and our licensure allows us to provide all forms of hormonal and non hormonal contraception. And the things that we don't do are really just the permanent options for contraception. So that means a vasectomy or a tubal ligation. Those are really the only two things that I can't offer to my clients, which is pretty awesome.
Imogen Raye Minton: God. That's so cool. Yasmeen, I just think that's such a smart system, you know, where you can really be a holistic care provider.
Yasmeen Bruckner: It really does feel as though it's providing continuity of care so that this person, this family that has entrusted you during their pregnancy and during their birth are then able to get what they need for the next phase. In the same place and from the same people. And I think that's really a service to the community. But to go to your question, which is what do I talk to people about - I talk to people about both non-hormonal options and progesterone-only options for people who are choosing to nurse their babies. I try to really tailor how I counsel people to what it is that they're in need of and what it is that they're looking to get out of their birth control. So I will say that for a lot of people, their goal is to prevent another pregnancy, maybe in the short term or maybe in the long term. And so if the goal is to consider having another baby relatively soon, then something like barrier methods, as Imogen spoke of it, can be really a nice option because they're not a long term commitment with something like a condom. Right? And you can choose whenever you're ready to stop using that, if you're wanting to conceive. I also offer people some progesterone-only option that's in a pill form. Again, that's a really nice choice because you can stop it at any time on your own. There are also IUD that I offer people in the postpartum period. I offer both the hormone-based IUD, because they have progesterone in them, and I also offer the copper IUD, or the non hormonal IUD, as well.
Rhea Ramjohn: So this is a really important conversation and I want to continue on this topic. But before we continue, we're going to take a quick break.
Hormonal is brought to you by Clue. The period tracking app, and menstrual health encyclopedia, and now, a pregnancy tracker!
You heard that correctly! Clue is launching our most requested feature ever: Clue Pregnancy mode! Now, you can track your pregnancy symptoms, get scientifically-backed information on how your body is changing each week, and follow your baby’s growth from conception to birth to post pregnancy.
If you’ve been using Clue as a period tracker, all you need to do is subscribe to Clue Plus, go to settings, and switch to Clue Pregnancy mode. Clue Pregnancy mode is available on Android today, and coming to Apple devices by the end of 2020.
Alright, back to the show.
Rhea Ramjohn: You're listening to hormonal. I'm Rhea Ramjohn.
You know, I’m curious about how the post-partum care differs between Germany and the US. Could you tell me a bit more about this? Imogen?
Imogen Raye Minton: Here in Germany, we have a really comparatively very, very supportive postpartum system where your midwife can visit you every day, every other day for multiple months, and you're protected by law to have at least two months postpartum off and, following up to a year and a couple months even beyond, paid for at least part of your original salary by the health insurance company and the government. And so there's a lot of support for people to be able to really rest during that period as much as you can rest when you have a baby and to allow this sort of process of your body returning to its nonpregnant state to happen in a healthy way. And I think that Yasmeen might experience that differently in the U.S., where there's really no strong federal postpartum protections. Is that the case?
Yasmeen Bruckner: That's really true. And it's actually... it's very challenging. We spend a lot of focus on pregnancy, but there is much less support here in the United States for postpartum care. There are no programs that allow people to be home more than maybe a couple of weeks. I live in a state where we're ahead of the curve or we're ahead of the rest of the country, I think, in having paid parental leave. Washington state now has a program for paid parental leave, which is about 12 weeks for most people. And either the birthing parent and the non birthing parent can take that time. But that is an anomaly here in this country. I work in a hospital setting. There are midwives who work at home and in birth centers. And so they will do home visits. But for my clients, I see them for a two week visit and a six week visit. More visits in between if needed. And then maybe a contraception visit after that. But then really in terms of support, that's it. Which is which is fine for some people, and it can also be really hard for others.
Rhea Ramjohn: So this is exactly why we find this conversation about midwifery and birth control interesting and the intersection of that, because as Imogen pointed out in Germany, you have so much postpartum care. It was the very first time that I had learned that midwives are a part of your postpartum care. I thought it all ended with the delivery of the baby. So thinking about that, and you've both mentioned this lifestyle post-delivery, this new addition to one’s lifestyle - what kind of advice would you give parents that they should know about their lifestyle, how that may change, and especially including birth control? At this time?
Imogen Raye Minton: I'm going to jump right in because I really like this topic. [Laughter] You know, my impression is we don't have a lot of very clear models of what early parenthood looks like. And I think that the models that we do have are incredibly hetero-normative and incredibly cis-normative.
I think that as our family has gotten more nuclear, we have less support structures. People are left more and more to their own devices in a situation where especially if -- and honestly, not to plug my job, but midwives are absolutely vital postpartum -- especially in contexts where they don't have midwifery support or, let's just say, any kind of knowledgeable regular guidance that they don't have to pay for out of pocket, but that's covered by insurance, I think that many people end up feeling incredibly overwhelmed. There's very high anxiety levels. There's higher chances of postpartum depression, both for the parent who gave birth and also for the parent that didn't or the parents that didn't. I think that also, if your family's structure doesn't fit into that kind of normative model, you might really struggle to figure out what you're supposed to be doing. You know, media isn't much help and online forums are a total wash. So I think that people feel really isolated. Sometimes! People can feel really isolated. They can feel like they don't have the information that they need to feel safe. And I think that, in combination with the fact that you're experiencing usually pretty significant sleep deprivation with a new baby, and if you're feeding the baby from your body, you're experiencing the effects of prolactin and also oxytocin when you are nursing or chest feeding or body feeding. These hormones are hormones that make you feel bonded and cuddly, they're not the kind of hormones that make you feel really enthusiastic about having -- everybody's different -- but having wild sex in the shower or something while the baby's sleeping, you know, I think a lot of people feel really touched out. I think a lot of people feel overwhelmed. And I think that those things are really normal.
But, in our culture, there's not a lot of conversation around it. And so I think that can feel really like you're faulty, like you're not functioning properly if you're not really enthusiastic about having sex postpartum. If your body doesn't feel familiar to you. If it feels like it's kind of at the beck and call of this other new little being, or if you feel like you're constantly doing chores and and other sort of reproductive work to support your partner who's busy feeding the baby, all of these things can create a situation where, for many people, contraception is not super high in their minds, but rather this feeling of pressure and disconnect surrounding sex and sexuality in general. I want to specify that while that's true for some, it's not true for others. Some people have super adventurous, very exploratory, fabulous sex lives shockingly quickly after giving birth. And that's fantastic, too. I just think that we don't talk about either of those things very much. And that's missing for me. That to me feels more important, having those conversations with my clients, separate from a conversation like... contraception is not more important to me than having that conversation about sexuality in general.
Rhea Ramjohn: So, Yasmeen, what do you recommend to people who are post-termination or post-miscarriage in terms of birth control? And how do you approach these conversations differently than, let's say, a pregnancy that leads to birth?
Yasmeen Bruckner: So I think the way that I start is a conversation about that person's fertility goals. We cannot assume that because somebody had a termination of pregnancy that that wasn't a desired pregnancy or that they don't desire pregnancy. And just because somebody has had a spontaneous miscarriage, it doesn't mean that that was a desired pregnancy either. So the first thing that I try really hard not to do is to make an assumption about where that person is and to have a conversation with them. What is it that you are hoping for? What is it that I can offer to you? Some people who've had a miscarriage, they don't feel ready to start trying right away. And so they do want something for contraception because while they may be ready to have sex again, they are not ready to start walking through the journey of pregnancy again. Other people who've had a miscarriage want to be able to try for pregnancy right away. And so in those situations, I don't counsel people that they have to wait or that they have to use contraception for three months or six months, which was kind of an old school thing that was happening in our country for reasons that are unclear to me. So I think that that's the approach I take: what is the goal? Somebody who doesn't want children right now, doesn't want a pregnancy right now, they have a whole range of choices. Every option is on the table for them, for contraception. And they can start that at the time of a miscarriage, at the time of a termination, so long as everything was normal and uncomplicated.
Imogen Raye Minton: I really agree with that. I just want to jump in there and say that I love the thing with this question, what kind of contraception do you recommend? You keep coming back to the answer: it's highly individual. And I think that is such an important tenet of many different kinds of health support. And I would say especially of midwifery care - IUDs are a good option for people who are in the position that Yasmeen was talking about, of really looking for a highly effective, longer term method with limited side effects. And I also am grateful that there is a method on the market that I can recommend where people can be so spontaneous, you know, if you decide that you don't want to be pregnant for four years and then, from Friday to Monday, you decide you do, you can have the IUD removed. And if it's a copper IUD, there are no lingering hormonal shifts. And for many people, it's possible to get pregnant immediately after removal. So it's a very flexible method.
Rhea Ramjohn: And I feel like we haven't explicitly said this, but from what I understand, people can get an IUD placed right away after a birth or maybe start the pill or another method right away after pregnancy. And also, when do these non-barrier methods come up?
Yasmeen Bruckner: I typically try to wait until the uterus is healed before initiating contraception, especially something like an IUD where there is the higher rate of the IUD coming out on its own if it's placed in the immediate postpartum period. But unfortunately, in our country, there are people who don't have great access to health care, or there are other barriers to getting health care in the postpartum period, and there are times where I do think that it is reasonable to give somebody an IUD immediately after the placenta comes out or to give somebody a birth control pill or birth control shot or an implant in their arm before they leave the hospital because they want contraception, they don't want to get pregnant right away, and they may not be able to come back for health care, or they may be in a situation where they could potentially get pregnant before they come back to get their contraception. So based on the setting that I work in, it's not something that I do often, but it is something that I do like to have the option that it can be really valuable for people.
Rhea Ramjohn: So we’re going to be doing a whole episode on Mythbusting on a future episode, but since you’re both so knowledgeable and have already busted some myths of my own today, and maybe just because I have it on the brain, I’m wondering if you both have myths you come across often that you’d like to bust and tell us the real deal? Do you have any myths?
Imogen Raye Minton: I think the myth that I'd most love to bust is that giving birth to a baby through the vagina somehow stretches you out and destroys your ability to feel pleasure. I think that that is such a pervasive myth for folks that they, in this stage of healing after birth, feel like one of the things that they're grieving is the loss of their previous sexuality. Like the way that things felt, the way that that clitoral stimulation feels, the way that penetration feels. And I just want to say that I have had equal experiences of folks who say their sexuality has blossomed postpartum and they have stronger orgasms that they can feel their whole clitoris, that they have much more focused pelvic floor control after they've done their wonderful pelvic floor classes and therefore can enjoy penetration in a different way. And I think another thing I want to point out is that some people have luck if they weren't previously able to ejaculate or squirt, doing that. And so there's just this incredible adventurous, you know, landscape ahead to explore either by yourself or with a partner or with multiple partners. And I think finding a method of having safer sex or using contraception that feels really empowering can be a very important part of making that feel fulfilling and satisfying.
Rhea Ramjohn: Oh, that's some of the best myth busting I've heard recently. Thanks for that! And Yasmeen, last but not least, what is a myth that you bust commonly?
Yasmeen Bruckner: Yeah. Yeah, such a good question. I have. I really try hard to bust the myth about “six weeks”, and I don't know if this is a myth in Germany, too. But there is this thing, this idea, that everything should be back to normal by six weeks. And I really try to encourage people to think about how long it took them to grow a baby in their body and the incredible feat it is to birth a baby no matter how you birth your baby. And then now for milk production to totally ramp up and be able to feed that baby, you know, maybe as the primary source of food for that baby, to just honor all of those transitions and to be kind to your body. I think the images that we get in the media of what women's bodies, what birthing people's bodies, should look like after they have a baby, six weeks later, is completely unrealistic. And it doesn't honor what the body's done. Some people are ready to have sex again, are ready to exercise again. But a lot of people are exhausted. Sex does not sound appealing, and that is totally 100 percent ok and normal.
Imogen Raye Minton: That's beautifully put.
Rhea Ramjohn: Wow. That’s perfectly said. I think that’s a great place for us to stop. I would like to say, Yasmeen Bruckner, who joined us from Seattle, Washington, Yasmeen is a certified nurse, midwife and women's nurse, health practitioner at the University of Washington Northwest Campus Midwives Clinic. Yasmeen, thank you so much for joining us.
Yasmeen Bruckner: Thank you so much for having me. It was a pleasure to be with you all this morning.
Rhea Ramjohn: And Imogen Raye Minton is a home birth midwife and co-founder of the Queer Feminist Midwifery Collective here in Berlin. Imogen joined us here in the studio, and thank you so much for joining us on the podcast as well.
Imogen Raye Minton: It's my pleasure. Thanks for hosting this.
Credits
Rhea Ramjohn: Hormonal is hosted by me, Rhea Ramjohn! Our Executive Producer is Kassandra Sundt.
Editorial help from:
Amanda Shea
Steph Liao
Nicole Leeds
Special thanks to:
Marta Pucci
Trudie Carter
Maddie Sheesley
Ryan Duncan
Aubrey Bryan
Claudia Taylor
Léna Calvarin
Lynae Brayboy
Yomi Eluwande
And Jane Parr-Burman
Mixing and recording help from Bose Park Productions and Rekorder Studios in Berlin.
Thanks for listening to Hormonal. Please rate and subscribe, and tell a friend! Until next time, I’m Rhea Ramjohn.
Related links:
https://helloclue.com/articles/life-stages/postpartum-sex-fertility-and-contraception
https://helloclue.com/articles/about-clue/how-to-use-the-clue-app-to-help-you-become-pregnant
https://helloclue.com/articles/pregnancy-birth-and-postpartum